Rise in Prostate Cancer Cases Contributes to Challenges in Care
Murugesan Manoharan, MD, FRACS, offers observations about prostate cancer care at Miami Cancer Institute.
Murugesan Manoharan, MD, FRACS

Troubling news about prostate cancer emerged from the American Cancer Society (ACS) in January. In its Cancer Statistics 2023 study1, published in the journal CA: A Cancer Journal for Clinicians, ACS scientists announced:
- The incidence of prostate cancer increased by 3 percent each year from 2014 through 2019.
- An estimated 288,300 new cases of prostate cancer will be diagnosed in the United States (US) in 2023, accounting for 29 percent of all new cancer cases in men.
- An estimated 34,700 men will die of prostate cancer this year, second only to lung and bronchus cancer as a cause of men’s cancer deaths.
- The incidence of prostate cancer is more than 70 percent higher in Black men than in White men.
These findings are due in part to the US Preventive Services Task Force’s 2012 recommendation to cease PSA screening in all men. Since then, early diagnosis and treatment of prostate cancer has dropped, while advanced prostate cancer cases have begun a steady rise.
I have observed several factors in play at Miami Cancer Institute as we respond to the challenge of prostate cancer.
Factors Contributing to Challenges in Prostate Cancer
Cost of PSA Screening
I concur with the ACS recommendation that men of all ages should have an opportunity to make an informed decision about whether prostate cancer screening is right for them. Balanced and unbiased counsel from the physician is vital. However, the cost of testing may be a barrier for some patients, as many insurance plans do not cover it. I have observed that wealthier patients in urban areas are more likely to have access to timely screening, while lower-income and minority individuals do not. The latter group includes many of my patients in the Haitian American community, who have a significant incidence of aggressive prostate cancer.
Plentiful Treatment Options
The array of prostate cancer treatments includes robotic surgery, external beam radiation including proton beam therapy, brachytherapy, cryotherapy, high-intensity focused ultrasound (HIFU), laser ablation, hormone and other drug therapy, chemotherapy, immunotherapy, and more. Direct-to-consumer marketing touting these various treatments can confuse and overwhelm patients. Again, careful consultation with an unbiased urologic oncologist is critical.
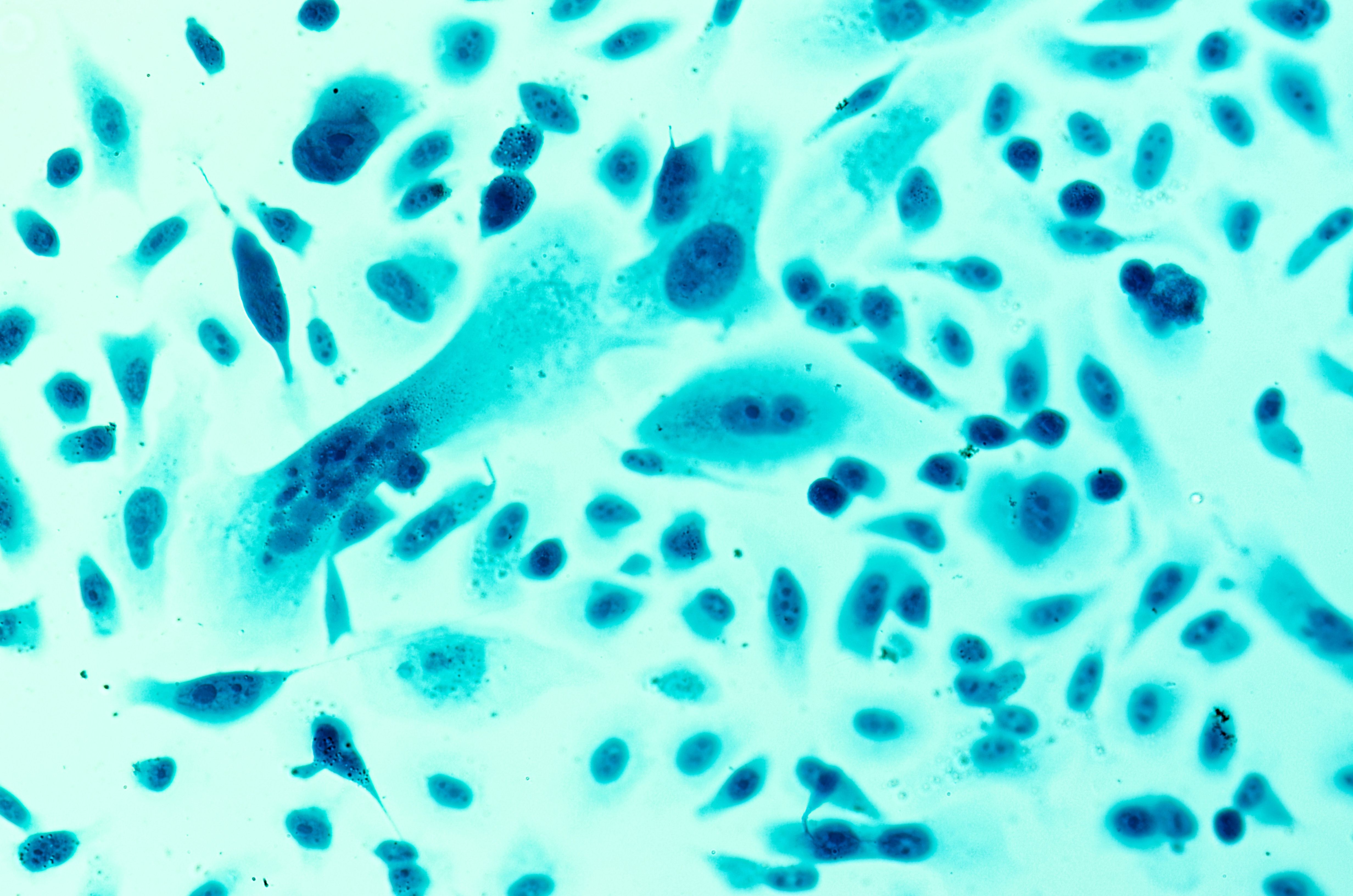
Image Credit © Sheitipaves [stock.adobe.com
FDA Reviews
While the US is quite advanced in prostate cancer treatment, The FDA’s ultra-cautious approach to approvals results in a lag in new-technology adoption.
For example, prostate specific membrane antigen (PSMA PET Imaging, which can accurately detect the spread of prostate cancer spread using a radioactive tracer, has been in use internationally since around 2014, but the FDA delayed its broad national approval of this technology until 2021.
High Intensity Focused Ultrasound (HIFU) therapy was studied as early as the 1940s and researchers focused on HIFU for the prostate in the 1990s. The treatment was approved in more than 20 countries, including Canada and Australia, before finally receiving FDA approval in 2015.
Last, the NanoKnife system, which employs low-energy, direct-current electrical pulses to destroy cancerous cells, was first made commercially available in 2009 but the FDA approved a pilot study only in 2019.
These technologies were widely used in cancer centers around the US prior to full FDA approval but since they weren’t covered by insurance, they were out of reach for many patients who could have benefited.
Addressing the Challenges in Prostate Cancer
Promoting Good Quality-of-Life
Death isn’t the only outcome of a prostate cancer diagnosis. The statistics don’t account for the pain, suffering, and inconvenience patients may endure while undergoing treatment. My team and I focus on helping patients maintain a good quality of life while we work towards a cure. Our patients express several priorities as they prepare for prostate cancer treatment:
A quick recovery: patients want to get back to work and everyday living. Technological advances such as minimally invasive surgery (sometimes with a single small incision) help make this possible. Many patients go home 24 hours after surgery. Once their pain can be managed without narcotics, they can usually resume driving and other daily tasks.
Reliable urinary function: patients frequently express concerns about incontinence. Twenty years ago, some 10 percent of patients were left incontinent by prostate surgery. Because we are now able to better protect the nerve bundles and urinary sphincter during surgery, 98 percent of patients do not need pads one year after surgery.
A healthy sex life: while measuring sexual potency is subjective, I advise patients that if they are potent before surgery, there’s a 75 to 90 percent chance they will remain potent after nerve-sparing surgery.
Managing treatment: traditional radiation treatments can require up to 6 weeks of daily hospital visits, a burdensome task for patients who are trying to hold down a job. Hyperfractionated radiotherapy uses higher doses of radiation spread over fewer days, allowing patients to keep a regular work schedule. Ablation therapy requires even less of a time commitment.
Novel treatment strategies
Novel treatment like theranostics are on the rise. Theranostics combines therapeutic, radioactive pharmaceutical particles with diagnostic imaging to examine cancerous cells. In prostate cancer patients, a PSMA PET scan is done to evaluate for metastatic disease. PSMA, or prostate-specific membrane antigen, is expressed by virtually all prostate cancers and its presence locates the cancerous cells accurately. When these cells and receptors are located, a theranostic medicine such as Lutetium-177 in combination with PSMA is administered, which binds to and kills the cancerous cells. Its use is currently limited to prostate-specific membrane antigen-positive metastatic castration-resistant prostate cancer.
Training
As prostate cancer diagnoses continue to rise, today’s physicians have a duty to prepare the next generation in the fight. Miami Cancer Institute, in concert with Florida International University’s Herbert Wertheim College of Medicine, offers a two-year Urologic Oncology fellowship covering all treatment modalities.
We also work with Year 3 and 4 medical students who haven’t yet chosen a specialty. It’s my job to introduce them to the challenges of our super-specialty and pique their interest in pursuing urologic oncological surgery.
Lastly, we support working physicians who desire to continue their education in the specialty. My colleagues and I offer surgical observation opportunities for local physicians as well as participate in international training programs.
The advent of teleconferencing has created exciting new training opportunities. We offer bimonthly telemedicine webinars through Baptist Urological Academy to an international audience. Many participating physicians and fellows become recognized urologic oncologists in their own countries.
Managing prostate cancer starts with screening and early diagnosis but extends into the effective management of prostate cancer. It requires constructive participation of all involved in the prostate cancer management including the government, health institutions, physicians, health care staff and most importantly, the patients.
REFERENCES
1, Siegel RL, Miller KD, Wagle, NS, and Jemal A, A. Cancer statistics, 2023. CA Cancer J Clin 2023; 73(1): 17- 48. doi:10.3322/caac.21763










