Quizartinib Plus Chemotherapy Emerges as Potential Option for FLT3-ITD-Mutant AML
Results from the phase 3 QuANTUM-First study create a position for quizartinib plus chemotherapy in the FLT3-ITD-positive acute myeloid leukemia armamentarium.
Harry Erba, MD, PhD

Overall survival (OS) improvement has been achieved by adding quizartinib to chemotherapy with or without allogenic hematopoietic stem cell transplant (allo-HSCT) vs chemotherapy and placebo for the treatment of adult patients with FLT3-ITD-positive, newly diagnosed acute myeloid leukemia (AML), according to published findings from the phase 3 QuANTUM-First trial (NCT02668653).1
“The addition of quizartinib to intensive induction and consolidation therapy and continued as a maintenance for up to 3 years significantly improves the survival of adults up to age 75 years old with FLT3 ITD-mutated AML who are eligible for intensive chemotherapy. The improvement in survival appears to be due to deeper remissions as measured by an FLT3 ITD measurable residual disease [MRD] assay, longer duration of complete remission, and lower cumulative risk of relapse,” Harry Erba, MD, PhD, hematologist/oncologist and professor of medicine, Hematologic Malignancies and Cellular Therapy, Duke Cancer Institute, told Targeted Oncology™.
The findings were from 539 patients, 268 of whom were treated with the quizartinib combination and 271 of whom received chemotherapy and placebo. Patients in the experimental arm received 2 cycles of quizartinib plus cytarabine and either daunorubicin or idarubicin with up to 4 cycles, as well as cytarabine consolidation followed by quizartinib of allo-HSCT. In the control arm, patients received 2 cycles of cytarabine and either daunorubicin or idarubicin followed by placebo, then 4 cycles of consolidation therapy. Treatment in the study continued for up to 36 cycles.2
Patients were followed to assess OS, the primary end point, as well as the secondary end points of event-free survival, complete remission (CR) rate, composite CR, composite CR with FLT3-ITD with MRD, and the number of patients with treatment-emergent adverse events (TEAEs).1,2
The median follow-up was 39.2 months (95% CI, 37.2-41.5 months) in the quizartinib arm and 39.2% (95% CI, 36.3-41.2 months) in the placebo arm. The median OS observed with quizartinib and chemotherapy was 31.9 months (95% CI, 21.0 months to not evaluable [NE]) compared with 15.1 months (95% CI, 13.2-26.2 months) in the placebo arm (HR, 0.78; 95% CI, 0.62-0.98; P = .032).1
The median relapse-free survival was 39.3 months (95% CI, 22.6 months-NE) with quizartinib/chemotherapy vs 13.6 months (95% CI, 9.7-23.7 months) with placebo (HR, 0.61; 95% CI, 0.44-0.85). Overall, the rate of relapse in the quizartinib plus chemotherapy arm was 30% vs 42% in the placebo arm, and the rate of death was 14% vs 17%, respectively.
Cumulative incidence of relapse was evaluated at 12 months, 24 months, and 36 months in both arms. Results showed that the cumulative incidence of relapse was higher with placebo compared with quizartinib at each time point.
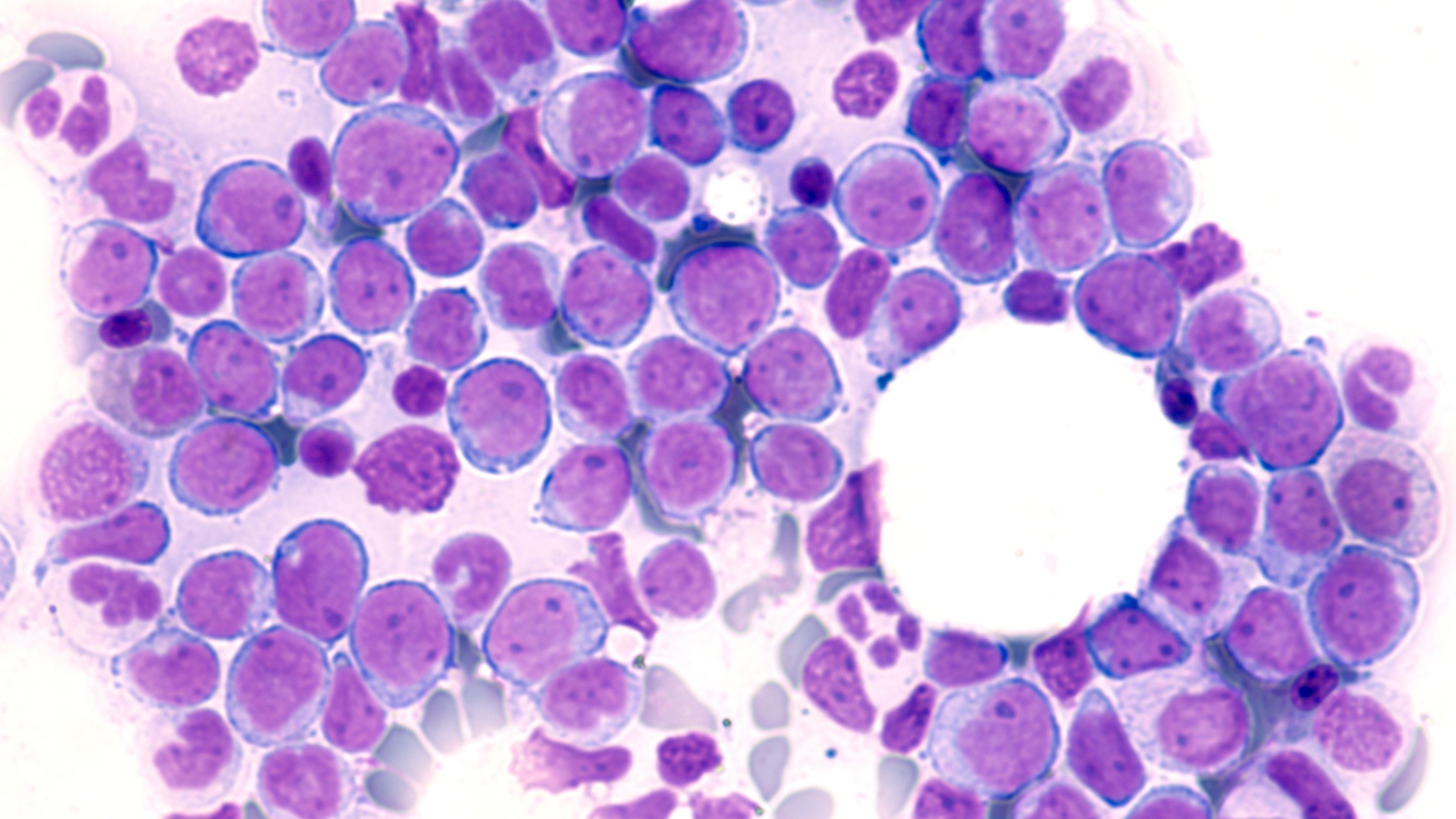
Image Credit: © David A Litman [stock.adobe.com]
CR rates were similar between the 2 treatment arms, according to Erba et al. Patients were exposed to therapy for a median of 10.71 weeks (IQR, 2.29-70.86 months) in the quizartinib arm and 9.50 weeks (IQR, 2.14-42.14 months) in the placebo arm. Overall, 72% of patients who were treated with quizartinib vs 65% of those given placebo had a CR after 1 or 2 cycles of induction therapy. Following induction therapy, 87% of the quizartinib arm vs 94% of the placebo arm went on to receive consolidation therapy. Quizartinib led to a longer median duration of CR. The median duration of CR was 38.6 month (95% CI, 21.9-NE) with quizartinib compared with 12.4 months (95% CI, 8.8-22.7 months) with placebo.
“The benefit of quizartinib, as measured by both the hazard ratio for the reduction in the risk of death in patients less than 60 years old, as well as the cumulative risk of relapse in the entire population, is superior to that reported with midostaurin [Rydapt] in the RATIFY trial [NCT00651261]. The QuANTUM-First trial only enrolled patients with the poor-risk FLT3 ITD mutations, whereas RATIFY included patients with FLT3 TKD [tyrosine kinase domain] mutations. Therefore, the prognostic impact of the FLT3 TKD mutation is not clear,” Erba explained.
All patients in the quizartinib arm experienced AEs vs 99% of the placebo arm. These events were grade 3 or higher in 92% of patients treated with quizartinib vs 90% of those in the placebo arm. TEAEs occurred in 60% of the quizartinib arm vs 36% of the placebo arm. Grade 3 or higher TEAEs were seen in 25% of the experimental arm vs 24% of the placebo arm.
Serious AEs occurred in 54% of the quizartinib arm compared with 46% of the placebo arm. The most common serious AEs were febrile neutropenia (11% v 8%), pneumonia (6% v 6%), and septic shock (4% v 3%). The most common any-grade AEs in the quizartinib arm vs the placebo arm were febrile neutropenia (44% v 42%), neutropenia (20% v 10%), and thrombocytopenia (11% v 11%).
Based on the QuANTUM-First findings, quizartinib has potential to be an effective and well-tolerated treatment option for FLT3-ITD-positive, newly diagnosed AML in patients between the ages of 18 and 75 years old, according to Erba et al.
“The majority of AML patients are not eligible for intensive chemotherapy based on advanced age, poor performance status and comorbid illnesses. Quizartinib has activity as a mono therapy in FLT3-ITD-mutated AML. There is minimal gastrointestinal toxicity with quizartinib,” said Erba. “QT prolongation has been associated with quizartinib, especially at higher doses explored in the phase I development of this agent. The risk of QT prolongation can be managed with attention to concomitant medications and monitoring, as we are accustomed to doing for many drugs used in oncology. Quizartinib needs to be evaluated as monotherapy and in combinations with less intensive therapy for patients who are not eligible for intensive therapy, both at diagnosis and at relapse,” he added.
REFERENCES:
1. Erba HP, Montesinos P, Kim H, et al. Quizartinib plus chemotherapy in newly diagnosed patients with FLT3-internal-tandem-duplication-positive acute myeloid leukaemia (QuANTUM-1. First): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. Published online April 25, 2023. doi:10.1016/S0140-6736(23)00464-6
2. Quizartinib with standard of care chemotherapy and as continuation therapy in patients with newly diagnosed FLT3-ITD (+) Acute myeloid leukemia (AML) (QuANTUM-First). ClinicalTrials.gov. Updated December 29, 2022. Accessed May 3, 2023. https://clinicaltrials.gov/ct2/show/NCT02668653?term=NCT02668653&draw=2&rank=1