Primary Debulking Surgery for Ovarian Cancer Riskier Than NACT-IDS Regimen
In a single-institution randomized prospective controlled trial of women with advanced epithelial ovarian cancer, 52.6% of patients in the PDS study arm had major complications with an MSKCC score of 3 or greater.
In a single-institution randomized prospective controlled trial of women with advanced epithelial ovarian cancer, 52.6% of patients in the PDS study arm had major complications with an MSKCC score of 3 or greater.
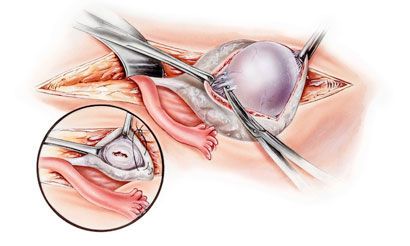
In a single-institution randomized prospective controlled trial of women with advanced epithelial ovarian cancer, 52.6% of patients (n=29) in the primary debulking surgery (PDS) study arm had major complications with an MSKCC score of 3 or greater. Patients in the other study arm received neo-adjuvant chemotherapy (NACT) followed by interval debulking surgery (61.1%, n=33), with a major postoperative complication rate of 6% (n=3). Postoperative mortality rates in the PDS group were 3.6% (n=2); no patients died in the interval debulking surgery (IDS) group, creating a statistically significant higher risk with the PDS protocol.
Lead author Anna Fagotti, MD, presented these findings on March 30, during the Late Breaking Abstract Session at the 2015 Society of Gynecologic Oncology’s (SGO) Annual Meeting on Women’s Cancer.
“The phase III SCORPION trial compared perioperative and survival outcome of PDS versus NACT followed by IDS in high tumor load advanced epithelial ovarian cancer patients,” said Fagotti, creator of the scoring method for predicting resectability and prognosis in advanced ovarian cancer that bears her name. “This study is an interim analysis with respect to SCORPION’s perioperative morbidity and mortality safety. There is a gray zone in which the best primary treatment option for patients is not clear yet.”
Fagotti is an assistant professor in the division of gynecological surgery at St. Maria Hospital, University of Perugia, Italy.
Eligible patients were 18-75 years old, had pathologically proven ovarian cancer, ECOG performance status of 0-2, a FIGO stage of IIIC-IV, no history of other cancers, and an intra-operative high tumor load assessed by staging laparoscopy (i.e., a Fagotti score of 8-12). Intra-operative mesenteral retraction and miliary carcinosis on the bowel were exclusion criteria. Patients were randomly assigned to the PDS or the NACT-IDS arm. Surgical data were evaluated by univariate analysis. Intra-operative and postoperative complications were assessed using the MSKCC surgical secondary events grading system. The data are too immature to assess median survival data in both arms at this time.
Between October 2011-November 2014, 200 women with suspected advanced epithelial ovarian cancer were enrolled, but only 110 were evaluable. The two groups showed no significant differences in preoperative characteristics and intra-operative tumor dissemination. In the patients who received upper abdominal surgery, 91% (n=50) of the PDS group and 90% (n=45) of the IDS group achieved optimal residual tumor (RT < or equal to 0.1cm), with a rate of complete cytoreduction (RT=0) of 45.5% (n=25) and 60% (n=30) respectively (P = 0.158).
Major postoperative complication rates (MSKCC score of 3 or greater) of the PDS and NACT-IDS groups were 52.6% (n=29) and 6% (n=3), respectively (P = 0.0001). The most common major postoperative complication was pleural effusion, with 31% (n=17) of PDS patients experiencing it, while only 1 IDS patient did. Additionally, 4 PDS patients developed sepsis and pulmonary thromboembolism occurred in 3 patients in this group. Only three major postoperative events in total occurred in the IDS group: 1 incidence was recorded of each of these: respiratory failure, pleural effusion and gastric bleeding. The most serious events occurred in the PDS group: 2 patients required re-operation with organ resection, 1 patient experienced multiorgan failure, and 2 patients died of acute cardiopulmonary failure, for a 3.6% postoperative mortality rate (P = 0.154).
The study team concluded that PDS is associated with a statistically significant higher risk of severe perioperative morbidity in patients with high tumor load advanced epithelial ovarian cancer compared to a NACT regimen followed by IDS (OR=19.3; CI=5.3-69.4). Most complications were of grade 3, with a higher incidence than that reported in previous retrospective studies.
The reported mortality rate of 3.6% corresponds to what has been previously reported in the literature (0.3%-5.7%).
“The pending survival data from SCORPION are needed to assess whether such an extreme complication rate is acceptable from a cost-effectiveness perspective,” said Fagotti. “While we continue to wait for the survival data, we should be very careful in choosing the primary approach in these specific circumstances for women outside a clinical trial.”
Fagotti A, Vizzielli G, Fanfani F et al. Phase III SCORPION trial (ID number: NCT01461850) in epithelial ovarian cancer patients with high tumor load receiving PDS versus NACT: ad interim analysis on peri-operative outcome. Presented at: 2015 Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer; March 28-31, 2015; Chicago, IL. Late Breaking Abstract.
<<<