Pirtobrutinib Shows Strong Efficacy in Recurrent CLL/SLL After BTK Inhibition
Results from the BRUIN study focusing on patients with chronic lymphocytic leukemia/small lymphocytic lymphoma showed benefit in patients were pretreated with Bruton tyrosine kinase inhibitors.
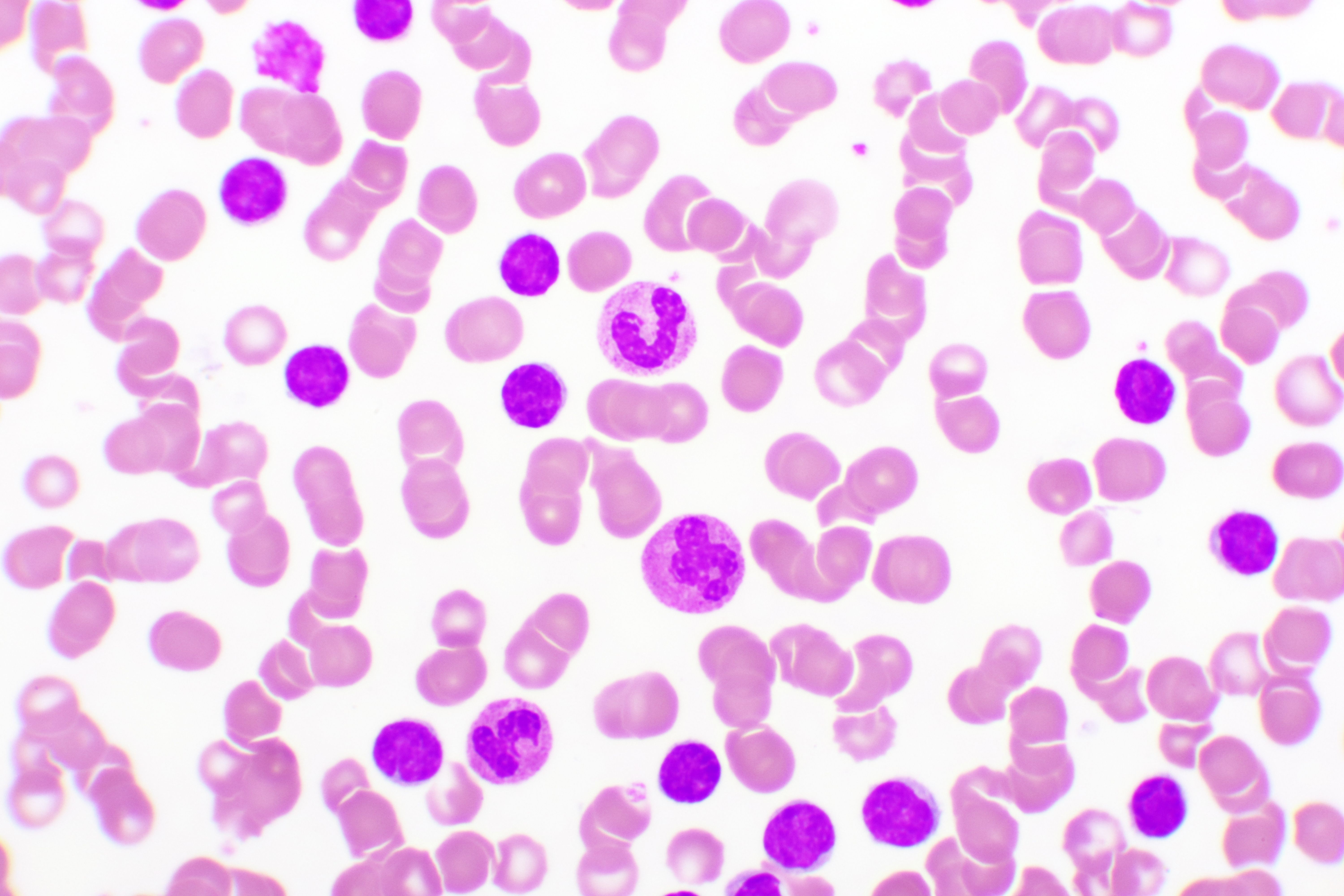
Image credit: © jarun011 via Adobe Stock
The Bruton tyrosine kinase (BTK) inhibitor pirtobrutinib (Jaypirca) demonstrated favorable overall response rate (ORR) and progression-free survival (PFS) in patients with chronic lymphocytic leukemia/small lymphocytic lymphoma previously treated with a covalent BTK inhibitor, according to results published in the New England Journal of Medicine.1
In the phase 1/2 BRUIN trial (NCT03740529), the ORR was 73.3% (95% CI, 67.3%-78.7%), with a median PFS of 19.6 months. Adverse events such as infection, bleeding, and neutropenia were common, but only 2.8% of patients discontinued treatment because of a treatment-related adverse event (TRAE).
“Patients with relapsed or refractory CLL or SLL following treatment with a covalent BTK inhibitor represent a population with limited treatment options,” Jennifer A. Woyach, MD, professor and hematologist-oncologist at The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute, the study's co-lead author, said in a press release.2 “These data support the potential for pirtobrutinib to extend the benefit of BTK inhibition for patients with CLL or SLL with a once-daily oral therapy.”
Covalent BTK inhibitors ibrutinib (Imbruvica), acalabrutinib (Calquence), and zanubrutinib (Brukinsa) are used to treat CLL, but they have a common resistance mechanism that limits their efficacy when used in sequence.1 The BCL2 inhibitor venetoclax (Venclexta), is also used as frontline or second-line therapy for CLL. Pirtobrutinib is a selective, noncovalent BTK inhibitor that is effective in both wild-type and C481-mutant BTK, which is associated with resistance to covalent BTK inhibition. It is approved for use in mantle cell lymphoma based on its efficacy in those patients in the BRUIN trial.3
The multicenter BRUIN trial enrolled patients at 49 sites in 10 countries. In the phase 1 portion, patients received doses ranging from doses ranging from 25 mg to 300 mg once daily, and in the phase 2 portion, they received 200 mg daily. The primary end point was overall response of partial response or better, with secondary end points including PFS and safety.
A total of 773 patients with B-cell cancers including 317 with relapsed or refractory CLL/SLL were enrolled in the trial.1 Of these, 247 had received prior BTK inhibitor including ibrutinib in 216, acalabrutinib in 44, zanubrutinib and nemtabrutinib in 7 each, vecabrutinib and spebrutinib in 3 each, and tirabrutinib in 1. Eighty-six were treated in the phase 1 portion and 161 were treated in the phase 2 portion.
The majority of patients previously treated with BTK inhibitor (76.9%) discontinued because of progressive disease, whereas 23.1% discontinued because of toxicity. Many patients had high-risk features such as deletion 17p, TP53 mutation, complex karyotype, or unmutated IGHV.
There were 176 partial responses, 1 nodular partial response, and 4 complete responses among the 247 who received prior BTK inhibitor. The rate of response including lymphocytosis was 82.2% (95% CI, 76.8%-86.7%). In 100 patients who had received both BTK inhibitor and venetoclax, the ORR was 70%, or 79% including those with partial response and lymphocytosis.
The overall median PFS was 19.6 months (95% CI, 16.9-22.1) at a median follow-up of 19.4 months. Median PFS was 16.8 months (95% CI, 13.2-18.7) in those who received prior BTK inhibitor and BCL2 inhibitor. In those who received only BTK inhibitor but not BCL2 inhibitor, the median PFS was 22.1 months (95% CI, 19.6-27.4). In patients who had received BTK inhibitor, BCL2 inhibitor, PI3K inhibitor, anti-CD20 antibody, and chemotherapy, the median PFS was 13.8 months (95% CI, 10.3-not estimable).
At a median follow-up of 22.6 months, the 12-month overall survival (OS) rate was 86.0% (95% CI, 81.0%-89.8%) and 18-month OS rate was 80.5% (95% CI, 74.8%-85.0%).
The safety population included 317 patients with CLL/SLL, 277 of whom had received at least 1 dose of pirtobrutinib at the recommended phase 2 dose of 200 mg daily. The median duration of treatment was 16.5 months.
The most common adverse event (AE) in the trial was infection in 71.0% of patients, followed by bleeding in 42.6%, and neutropenia in 32.5%. Infection of grade 3 or higher occurred in 28.1% and neutropenia of grade 3 or higher was reported in 26.8%. The rate of grade 3 or higher neutropenia associated with treatment with pirtobrutinib was 14.8%. Sixteen patients died for reasons besides disease progression, including 8 due to COVID-19, 2 due to pneumonia or fungal pneumonia, 2 due to septic shock or shock, and 4 for other causes.
Dose reductions due to treatment-related AEs were only required in 15 patients (4.7%), and discontinuation of pirtobrutinib was needed in 9 patients (2.8%).
The overall trial population including patients with other B-cell malignancies was similar, though the rate of infection was only 55.6% across all cancers.
"We are pleased to have the detailed safety and efficacy results of pirtobrutinib in adults with CLL or SLL published in NEJM and shared with the broader medical community," said David Hyman, MD, chief medical officer of Loxo@Lilly, the oncology unit of Eli Lilly and Company.2 "Treating clinicians have expressed the desire to fully exhaust BTK inhibition prior to switching their patients to another therapy class. These data continue to reinforce pirtobrutinib's ability to help reestablish BTK inhibition following treatment with a covalent BTK inhibitor."
References:
1. Mato AR, Woyach JA, Brown JR, et al. Pirtobrutinib after a covalent BTK inhibitor in chronic lymphocytic leukemia. N Engl J Med. 2023;389(33-44). doi:10.1056/NEJMoa2300696
2. New England Journal of Medicine Publishes BRUIN phase 1/2 trial data for pirtobrutinib in BTK inhibitor pre-treated adult patients with chronic lymphocytic leukemia or small lymphocytic lymphoma. News release. Eli Lilly and Company. July 6, 2023. Accessed September 13, 2023. https://tinyurl.com/y9ebbn5k
3. FDA grants accelerated approval to pirtobrutinib for relapsed or refractory mantle cell lymphoma. News release. FDA. January 27, 2023. Accessed September 13, 2023. https://tinyurl.com/23h93vf2
Selection of Next-Gen BTK in CLL Limited By Lack of Direct Comparison
February 4th 2025During a Case-Based Roundtable® event, Nakhle Saba, MD, and participants discussed the data supporting the 2 newer BTK inhibitor therapies acalabrutinib and zanubrutinib in patients with chronic lymphocytic leukemia who received 1 prior line of therapy in the second article of a 2-part series.
Read More