Phase 1/2 Trial of Olaptesed Pegol Shows Potential in Glioblastoma
The CXCL 12 inhibitor delivered a 50% overall survival rate at 18 months in the GLORIA trial, and its manufacturer intends to seek FDA guidance on further trial design.
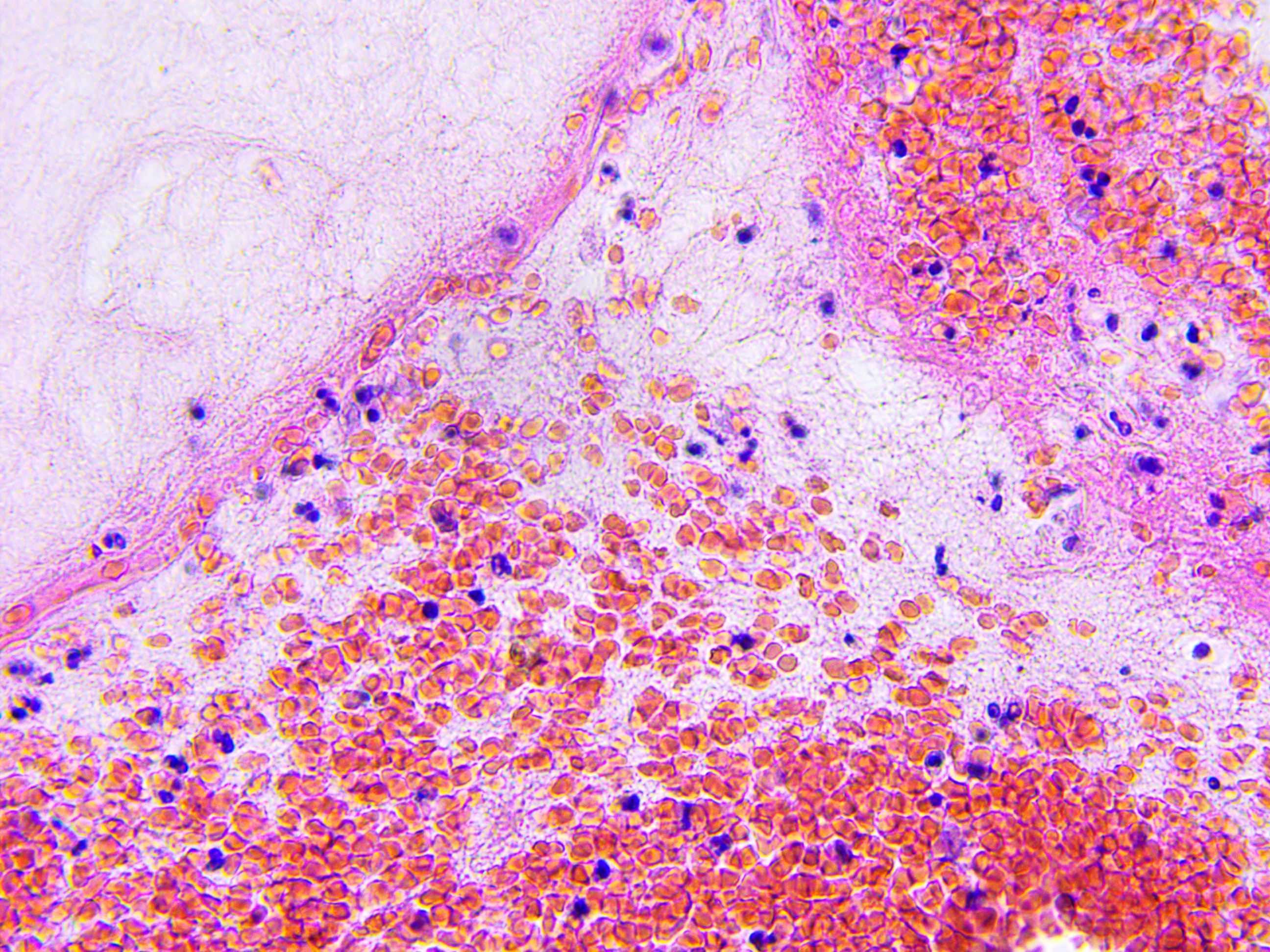
Brain tissue microscopic photography: ©lukszczepanski - stock.adobe.com
Olaptesed pegol (NOX-A12), a CXCL12 inhibitor, shows potential as a treatment for adult patients with glioblastoma (GBM) when used in combination with bevacizumab (Avastin), a VEGF inhibitor, and radiotherapy.1
Findings from the phase 1/2 GLORIA (NCT04121455) study show an overall survival (OS) rate of 50% at 18 months after the start of therapy. This number is expected to increase to 67% after the next patient reaches 18 months of survival. In contrast, 5% of patients receiving the standard of care for GBM reached 18 months after treatment initiation, according to a press release from TME Pharma, study sponsor and manufacturer of NOX-A12.1
With these findings, TME Pharma announced its intentions to seek guidance for subsequent trial design from the FDA in the coming months. The company also intends to seek fast-track designation from the FDA and submit an investigational new drug application for olaptesed pegol for GBM in the first quarter of 2024.
“We believe that having a clear path to marketing approval in brain cancer, validated by FDA, will significantly increase the attractiveness of NOX-A12 to investors and potential partners,” said Aram Mangasarian, chief executive officer of TME Pharma, in a press release. “We anticipate that an additional trial or an expansion of the upcoming trial would be required for full approval.”1
The GLORIA study’s primary end point is to evaluate safety and treatment-related adverse events. The secondary end points include progression-free survival (PFS) at 6 months, median PFS, median OS, quality-of-life, and neurologic functions. The study is broken down into dose-escalation and -expansion cohorts.
The study enrolled 27 patients over the age of 18 years with newly diagnosed, histologically confirmed, supratentorial WHO grade IV GBM. To be eligible for the dose-escalation cohort, patients must agree to subcutaneous port implantation and have a maximum ECOG score of 2. Eligibility criteria for the expansion cohort are the same as the dose-escalation cohort, plus patients must have unmethylated MGMT promoter status and an estimated minimum life expectancy of 3 months.
Exclusion criteria for the dose-escalation cohort includes chemotherapy within the past 5 years, prior radiotherapy to the head, pregnancy, lactation, and uncontrolled intercurrent illness. Patients with history of other cancers are also excluded, except for patients with history of adequately treated basal of squamous cell skin cancer, in situ cervical cancer, or other cancer from which they have been disease-free for over 5 years.
Exclusion criteria for the dose-expansion cohort is the same as that of the dose-escalation cohort, plus any contraindications to MRI contrast agents or any of the drugs administered in the study, clinically significant or uncontrolled cardiovascular disease, history of arterial or venous thrombosis, hypersensitivity to monoclonal antibodies, evidence of metastasis to the central nervous system, and evidence of intracranial or intra-tumoral hemorrhage.
In experimental cohort 1, patients are receiving 200 mg of olaptesed pegol for 26 weeks administered intravenously plus radiotherapy weeks 1-6. Experimental cohort 2 receives the same treatment but with 400 mg of olaptesed pegol, and the experimental cohort 3 receives 600 mg of olaptesed pegol.
Expansion group A receives 600 mg of olaptesed pegol for 26 weeks, radiotherapy for weeks 1-6, and 10 mg/kg of bevacizumab every 2 weeks for 26 weeks. Expansion group B receives 600 mg of olaptesed pegol for 26 weeks plus radiotherapy for weeks 1-6. Expansion group C receives 600 mg of olaptesed pegol for 26 weeks, radiotherapy for weeks 1-6, and 200 mg of pembrolizumab (Keytruda) every 3 weeks for 26 weeks.
The study has an estimated completion date of December 2024.2
REFERENCES
1. TME Pharma provides positive update on 18-month survival for NOX-A12 combination regimen in brain cancer and provides strategic update including decision to engage with US FDA. TME Pharma. News release. October 10, 2023. Accessed October 11, 2023. https://tinyurl.com/558sx5j9
2. Glioblastoma treatment with irradiation and olaptesed pegol (NOX-A12) in MGMT unmethylated patients (GLORIA). ClinicalTrials.gov. Updated June 22, 2023. Accessed October 11, 2023. https://clinicaltrials.gov/study/NCT04121455
FDA Approves FoundationOne CDx as Companion Diagnostic for Tovorafenib in Pediatric Low-Grade Glioma
January 17th 2025FoundationOne CDx is now FDA-approved as the first companion diagnostic for tovorafenib, enabling targeted treatment for relapsed/refractory pediatric low-grade glioma with BRAF mutations or rearrangements.
Read More