Optimizing Autologous Stem Cell Transplant Protocols in Myeloma
Balancing cost and efficiency remains at the crux of autologous stem cell transplants for multiple myeloma treatment.
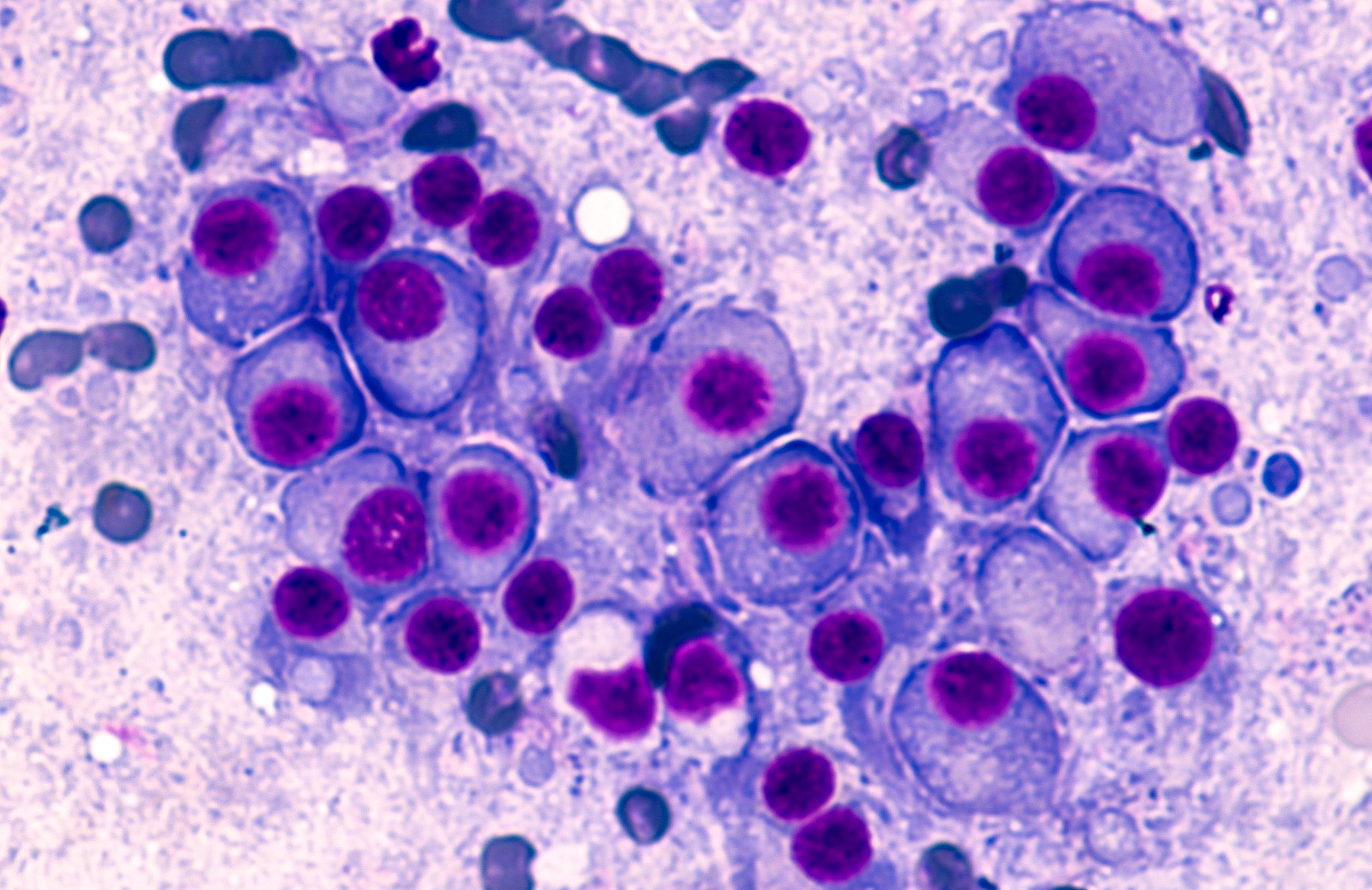
Multiple Myeloma: © David A Litman - stock.adobe.com
March is Multiple Myeloma Awareness Month. This month, Targeted Oncology is highlighting research in the field of myeloma treatment.
While new agents have emerged to improve the process of mobilization and collection for autologous stem cell transplantations for the treatment of multiple myeloma, standardized practices of these agents have still not reached a consensus. There are many factors to consider when using these agents, but the biggest 2 remain cost and time.
Researchers at the Cleveland Clinic, including Daniel Cancilla, MD, sought to get closer to identifying the best way to use agents like plerixafor, a mobilizing agent to facilitate the stem cell collection process. While plerixafor is an effective drug, it is also expensive.
The study aimed to reduce plerixafor use and its costs by updating the criteria for starting the agent. Previously, patients received plerixafor if they met any of 4 criteria. The new criteria require meeting all of the following: being aged 65 or older, having received 6 or more cycles of lenalidomide (Revlimid), and having a platelet count of 100,000 or lower. If collection counts were unsatisfactory, plerixafor could then be administered.
While plerixafor usage before the first collection significantly decreased, the overall plerixafor use per patient decreased slightly but remained statistically significant.However, the number of apheresis sessions needed per patient significantly increased.
These findings suggest a trade-off between plerixafor cost and procedure burden. Future research may explore further refinements to protocols for the optimal balance between cost and efficiency.
In an interview with Targeted Oncology, Cancilla, second-year internal medicine resident at the Cleveland Clinic, further discussed the study and its findings that were presented at the 2024 Transplantation and Cellular Therapy Tandem Meetings.
Targeted Oncology: What was the rationale for this study?
Cancilla: We are looking at this as a resource utilization analysis, looking at our institutional algorithm for stem cell collection, specifically for multiple myeloma. What we are looking at is the use of this drug plerixafor. Plerixafor has been shown to augment mobilization to collect stem cells for transplant.However, it is quite expensive, so there's this trade off trying to maximize our collections and minimize the time it takes to do that, but also conserving this quite expensive resource.
The impetus for this study is a few years ago in to conserve on our use of plerixafor, we changed some of our institutional algorithm to reduce the amount of plerixafor we use upfront. We wanted to see, number 1, did this save on the amount of plerixafor we use, and number 2, did this end up increasing the amount of time it would take us to collect the appropriate number of stem cells?
What are some of the unmet needs in this space?
Plerixafor is not brand new by any means, but it is a relatively new drug in the arsenal of mobilizing agents. Still, there are no standardized guidelines or universally accepted protocol for the mobilization process. These practices vary quite widely across different institutions. We are at a large center where we are doing a lot of these transplants and mobilizations [and] sharing our data with our 2 different types of mobilization regimens that we use can add to this growing body of literature and, hopefully, maybe just get a few steps closer to a more standardized protocol.
Can you summarize the findings?
The goal in the change of protocol was to reduce the amount of plerixafor we gave upfront, so that was very much achieved. Before this change, maybe 80% to 90% of patients were getting plerixafor upfront. After the change, maybe under 20% were getting the plerixafor upfront. That was completely unsurprising.
What was maybe more surprising was that ultimately, the amount of plerixafor we used was not decreased so much. What would happen is patients would mostly not get plerixafor, and then their collection yield would be not quite adequate, so they would have to get it for subsequent collection sessions. There was a significant drop in the amount of plerixafor, much less than we expected.
What did go up more significantly with the amount of time it took for patients to collect their stem cells. On average, [this was] from a little north of 1 apheresis session per patient up to north of 2.
The results are a little preliminary, but based on our initial assessment, it seems maybe the benefits did not outweigh the costs, especially when [we] factor in the cost of the apheresis sessions.
Are there any takeaways from these findings?
I think the big takeaway is that there are these new drugs out that have greatly boosted our ability to help collect these stem cell. The process can be done usually in a couple of days. Looking at these patients’ data, oftentimes the adverse effects, at least associated with mobilization, are pretty minimal. Most patients tolerate this well. Something I would say to community oncologists is that you can reassure your patients that the collection is a relatively safe process. With developments in recent years, the time it takes to do this has gotten shorter and shorter.