Metformin Use in Patients With Breast Cancer and Diabetes Improves Survival
A recent meta-analysis published in The Oncologist found that metformin use in patients with simultaneous diabetes and breast cancer improved overall survival (OS) and cancer-specific survival.
A recent meta-analysis published inThe Oncologistfound that metformin use in patients with simultaneous diabetes and breast cancer improved overall survival (OS) and cancer-specific survival, as well as improved OS by 65% after adjusting for hormone receptor expression.1
The authors cited evidence indicating the anticancer nature of metformin, which entails preclinical work and clinical trials.1-4However the authors also stated that a recent meta-analysis of metformin use in patients with both type 2 diabetes and different types of cancers failed to show an advantage against breast cancer in the subanalysis. This could be potentially due to the small sample size.5Another meta-analysis was performed specifically geared toward metformin use in breast cancer patients, with or without diabetes.
The multidisciplinary team of authors, which included oncologists and epidemiologists, conducted a broad literature search of several databases from inception of the data to January 10, 2015.1The search included:
- PubMed
- Embase
- Web of Science (Thomson Scientific)
- China Knowledge Resource Integrated Database
- VIP Journal Integration Platform
- Chinese Biomedical Literature databases
The research team sought out abstracts and papers that examined the relationship between metformin use and outcomes in patients with breast cancer.1Metformin exposure was defined as either “ever or currently taking metformin at the diagnosis of cancer,” or “taking metformin after cancer diagnosis.” Specifically they looked for papers that evaluated any prognostic outcome by metformin use, evaluated a breast cancer patient population, or contained original data analysis.
Literature that included these characteristics were used for the study if they also contained all-cause, cancer-specific mortality or OS, risk estimate (HR) relating use of metformin to death by employing survival analysis regression models, included standard error (SE), or 95% confidence intervals (CI).
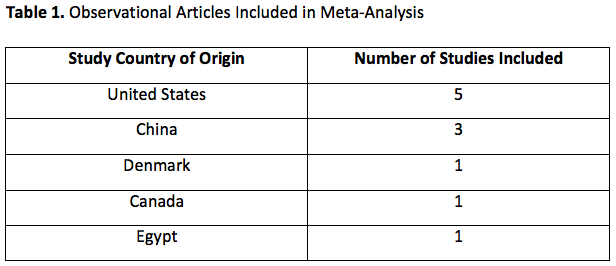
The authors retained 234 abstracts and 65 articles of the 2751 titles evaluated. After applying their criteria, 11 observational articles were included in the meta-analysis and were of international origin (Table 1). In 10 of the studies, quantitating metformin exposure was the primary goal, while one study included metformin exposure along with a range of prognostic variables. These studies provided data for a total of 5464 patients with breast cancer and diabetes. Of these, 2760 patients received metformin, and 2704 did not.1
The median number of patients per study was 141 (range, 39-236). The baseline used to calculate survival was from the time of cancer diagnosis, or date of surgery in studies containing surgical cohorts. Diabetes was diagnosed by blood tests and/or medical records.1
All-Cause Mortality, Cancer-Specific Mortality, and Metformin
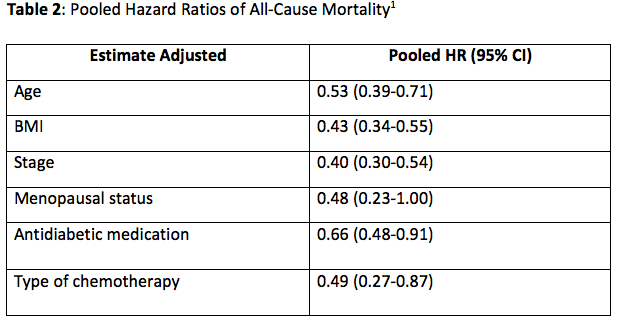
The meta-analysis found that taking metformin for diabetes was associated with a 47% reduced risk of death from all causes in patients with breast cancer (HR, 0.53; 95% CI, 0.39-0.71). The authors conducted a sensitivity analysis due to the large variations in the covariates in each study.
After adjusting for hormone receptor expression in malignant tissue, metformin use was associated with the biggest decrease in the risk of death (65%; HR, 0.35; 95% CI, 0.15-0.84). Other pooled HRs (95% CI) of all-cause mortality in the breast cancer patient population studied, with and without metformin are listed inTable 2.1
The pooled HR (95% CI) for the studies evaluating metformin use after cancer diagnosis was 0.64 (0.45-0.90). There was a lower risk of cancer-specific death for patients who took metformin versus those who did not receive the treatment (HR, 0.89; 95% CI, 0.79-1.00).1
Comparing Patients With and Without Diabetes
When comparing data for patients with breast cancer with diabetes taking metformin with those without, patients taking metformin had a significantly lower risk of all-cause mortality (HR, 0.63; 95% CI, 0.51-0.78). The paper stated that often patients with diabetes, especially if severe, are given less vigorous anticancer regimens due to the metabolic consequences of diabetes adversely affecting response to anticancer therapy. Yet, the analysis shows there was still a survival advantage associated with metformin use compared with patients with breast cancer who do not have diabetes.1
Additional Points
The authors wrote that one of the strengths of the study was the large number of patients. A post-hoc power calculation that confirmed their meta-analysis had a 98.6% power to demonstrate an association between metformin use and overall cancer mortality.
Finally, the authors stated that there is currently a need for prospective studies to validate metformin use as a prognostic factor, and the concept of an antidiabetic regimen included in the treatment of breast cancer.1
References
- Xu H, Chen K, Jia X, et al. Metformin use is associated with better survival of breast cancer patients with diabetes: a meta-analysis.Oncologist. 2015;20(11):1236-44. doi: 10.1634/theoncologist.2015-0096.
- Ben Sahra I, Laurent K, Loubat A, et al. The antidiabetic drug metformin exerts an antitumoral effect in vitro and in vivo through a decrease of cyclin D1 level.Oncogene. 2008;27(25):3576-86. doi: 10.1038/sj.onc.1211024.
- Jiralerspong S, Palla SL, Giordano SH, et al. Metformin and pathologic complete responses to neoadjuvant chemotherapy in diabetic patients with breast cancer.J Clin Oncol. 2009;27(20):3297-302. doi: 10.1200/JCO.2009.19.6410.
- Lee JH, Kim TI, Jeon SM, Hong SP, Cheon JH, Kim WH. The effects of metformin on the survival of colorectal cancer patients with diabetes mellitus.Int J Cancer. 2012;131(3):752-9. doi: 10.1002/ijc.26421.
- Yin M, Zhou J, Gorak EJ, Quddus F. Metformin is associated with survival benefit in cancer patients with concurrent type 2 diabetes: a systematic review and meta-analysis.Oncologist. 2013;18(12):1248-55. doi: 10.1634/theoncologist.2013-0111.