Melanoma: An Increasing Threat
Skin cancer is the most common form of malignancy in the United States, and melanoma represents the most deadly subset.
1Although melanoma represents less than 10% of all skin cancers, it is one of the fastest growing cancers and accounts for more than 75% of skin cancer-related deaths,2with the median survival for patients with stage IV melanoma ranging from 8 to 18 months after diagnosis (Figure).3It is estimated that approximately 1 in 74 Americans will be diagnosed with the disease, with the median age at diagnosis of 57 years.1
Figure. Cancer Mortality Rates by State: Melanoma
Cancer Mortality Rates by State: Melanoma
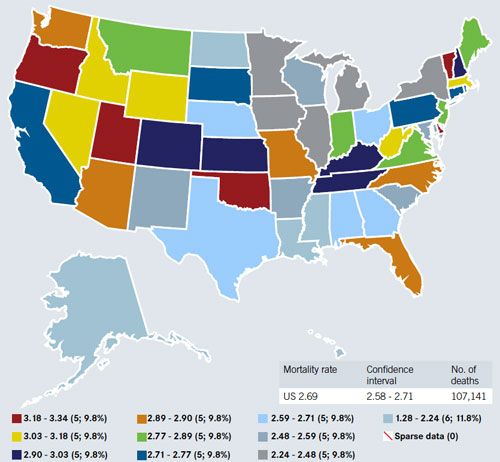
*Age-adjusted 2000 US population; white and nonwhite and both sexes, 1990-2004, all ages. Source: ratecalc.cancer.gov
Melanoma is diagnosed more commonly in Caucasians than non-Caucasians. In addition to white skin, other risk factors for melanoma include a personal history of nonmelanoma skin cancer, family history of melanoma, the presence of dysplastic and multiple nevi, large congenital nevi, light eyes, fair hair, tendency to freckle, sun sensitivity, and immunosuppression. Intermittent, intense sun exposure, as well as exposure to the sun during childhood, and more than one blistering sunburn in childhood are also associated with an increased risk of melanoma, although the neoplasm can develop in areas of the skin that do not receive sun exposure.1,4Although an association between inflammatory bowel disease (IBD) and increased risk of nonmelanoma skin cancers is well established, an association with melanoma has only recently been demonstrated, highlighting the need for routine screening of patients with IBD for skin cancer.4Most cases of melanoma are diagnosed at a localized stage, and have a high 5-year survival rate (greater than 95%), but the rates decrease markedly in patients with regional (61.7%) and distant (15.2%) metastases, for whom the prognosis is poorer.5
The mitogen activated protein kinase (MAPK) pathway is frequently activated in human cancers, leading to malignant phenotypes such as autonomous cellular proliferation. One important breakthrough in understanding the pathogenesis of melanoma is the discovery that this is the key signaling pathway in melanoma development. In normal cells, the tightly regulated pathway transmits extracellular signals from the cell membrane to the nucleus via a cascade of phosphorylation reactions. The pathway comprises RAS, RAF, MEK1/2, and ERK1/2, which sequentially transmit proliferative signals from cell surface receptors to the nucleus via cytoplasmic signaling. The MAPK pathway is dysregulated in most melanomas due to activating mutations in theBRAFandRASgenes, or other genetic or epigenetic modifications, which enhance signaling activity, thereby promoting cell proliferation, invasion, metastasis, migration, survival, and angiogenesis. Approximately 60% of the more common forms of melanoma involve BRAF mutations.RASmutations occur in 15% to 30% of cutaneous melanomas, and are mutually exclusive ofBRAFmutations. Not surprisingly, this signaling pathway therefore represents an important therapeutic target for the treatment of melanoma.1,6
However, despie developments in drug discovery and advances in molecular approaches for identification of drug targets, both the incidence of melanoma and its associated mortality rate continue to increase significantly, and faster than the rate with other cancers.5,7-9Between 1950 and 2000, the incidence of melanoma increased by more than 600%, and it is predicted to continue to become an increasing public health problem in the future.2
One major reason for the poor prognosis in patients with advanced melanoma is that there are few treatment options available for them. In the recent decade, there were no new FDA approvals for novel treatments for advanced melanoma until the 2011 approvals of the BRAF inhibitor vemurafenib and the immunomodulatory antibody ipilimumab, both of which dramatically changed the treatment landscape for patients with advanced melanoma.6
References
- Evans MS, Madhunapantula SV, Robertson GP, et al. Current and future trials of targeted therapies in cutaneous melanoma. WS El-Deiry (ed). Impact of Genetic Targets on Cancer Therapy.Adv Exp Med Bio. 2013;223-255.
- Kwong LN, Davies MA. Targeted therapy for melanoma: rational combinatorial approaches.Oncogene. 2013;1-9.
- Chapman PB, Hauschild A, Robert C, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation.N Engl J Med. 2011;364(26):2507-2516.
- Singh S, Nagpal SJS, Murad MH, et al. Inflammatory bowel disease is associated with an increased risk of melanoma: a systematic review and meta-analysis.Clin Gastroenterol Hepatol. May 2, 2013 [Epub ahead of print].
- Pretto F, Neri D. Pharmacotherapy of metatstatic melanoma: emerging trends and opportunities for a cure.Pharmacol Ther. May 2, 2013 [Epub ahead of print].
- Nikolaou VA, Stratigos AJ, Flaherty KT, et al. Melanoma: new insights and new therapies.J Invest Derm. 2012;132:854-863.
- Madhunapantula SV, Robertson GP. Chemoprevention of melanoma.Adv Pharmacol. 2012;65:361-398.
- Garbe C, Eigentler TK, Keilholz U, et al. Systematic review of medical treatment in melanoma: current status and future prospects.Oncologist. 2011;16:5-24.
- Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma.N Engl J Med. 2010;363(8):711-723.