Improved RFS in Resected Melanoma with mRNA Vaccine/Pembrolizumab
Pembrolizumab and mRNA-4157 demonstrated improvements in subgroups of resected melanoma, including those with BRAF-mutated tumors, in the phase 2 KEYNOTE-942 trial.
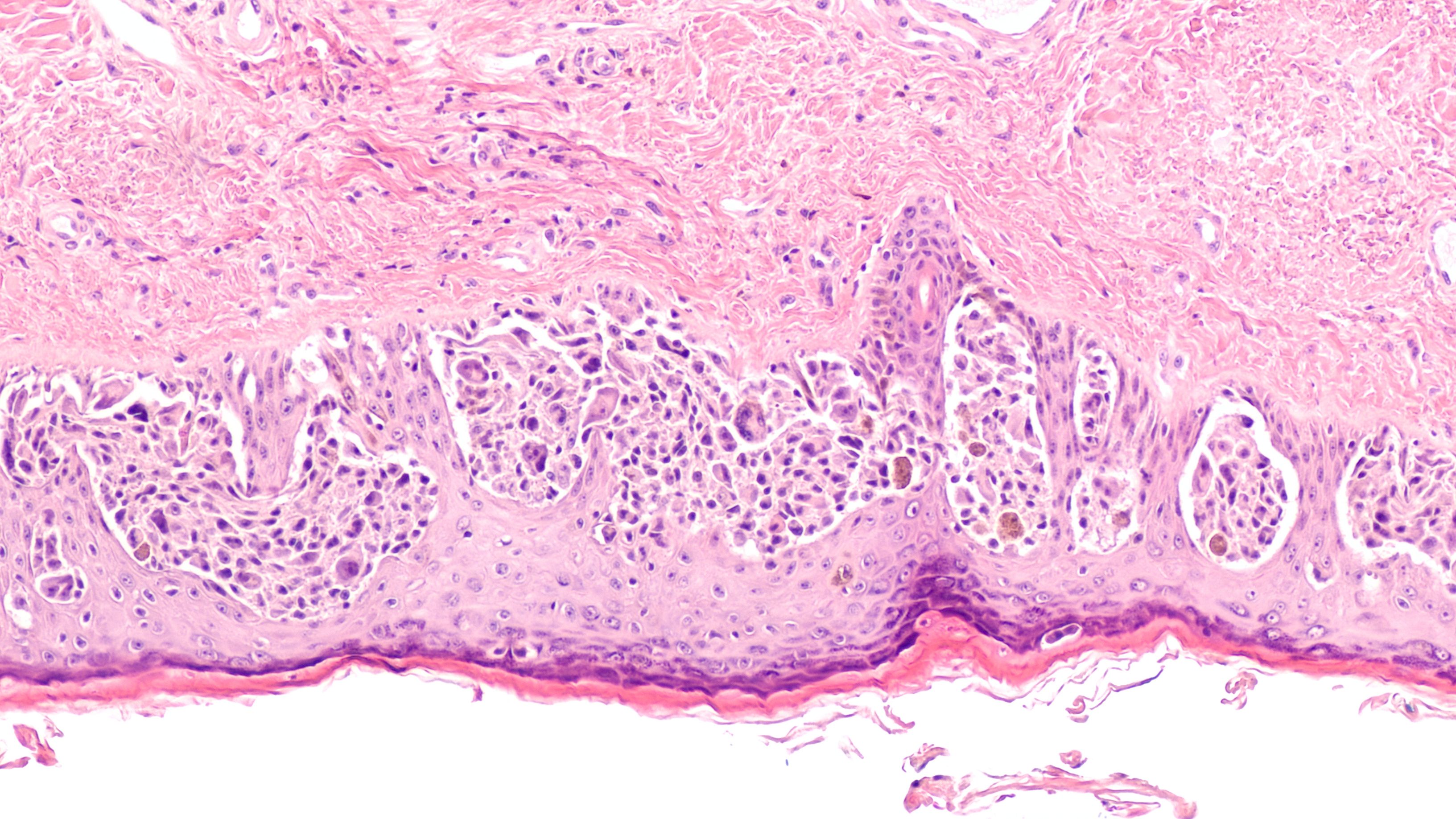
Melanoma: © David A Litman - stock.adobe.com
Combining the individualized neoantigen therapy mRNA-4157 (V940) with pembrolizumab (Keytruda) yielded clinically significant improvements in distant metastasis-free survival (DMFS) and relapse-free survival (RFS) compared with pembrolizumab monotherapy in patients with high-risk resected melanoma, according to findings from the phase 2 KEYNOTE-942 trial (NCT03897881) presented at the 2023 European Society for Medical Oncology Congress (ESMO).
Patients treated with mRNA-4157 plus pembrolizumab experienced an approximately 44% reduction in the risk of death or recurrence with respect to RFS compared with those receiving pembrolizumab alone (HR, 0.561; 95% CI, 0.309-1.017; P = .0266). Additionally, the RFS rates in the combination and monotherapy arms, respectively, were 83.4% vs 77.1% at 12 months and 78.6% vs 62.2% at 18 months.
The individualized neoantigen therapy in combination with pembrolizumab also improved DMFS compared with pembrolizumab monotherapy (HR, 0.347; 95% CI, 0.145-0.828; P = .0063). The 18-month DMFS rate was 91.8% in the mRNA-4147 plus pembrolizumab arm and 76.8% in the single-agent pembrolizumab arm.
Among patients who were circulating tumor DNA (ctDNA) negative, the experimental combination produced improvements with respect to RFS (HR, 0.225; 95% CI, 0.095-0.531) and DMFS (HR, 0.048; 95% CI, 0.006-0.380). It was also reported that RFS and DMFS outcomes improved among patients who were ctDNA positive and received the combination compared with those who received single agent pembrolizumab.
“The baseline ctDNA status may have prognostic value,” Jeffrey Weber, MD, PhD, a medical oncologist and deputy director of the Perlmutter Cancer Center at NYU Langone Health, said during the presentation. When breaking patients into different longitudinal patterns over time, those who were ctDNA negative (n = 112) achieved the lowest recurrence rate (17%), whereas those who were ctDNA molecular non-responders (n = 16) experienced the highest recurrence rate (94%).
Developers designed mRNA-4157 as a customizable, individualized neoantigen therapy encoding a maximum of 34 neoantigens. It is hypothesized that neoantigen-targeting therapies may enhance endogenous neoantigen T-cell responses and enable epitope spreading to novel antigens that may drive antitumor responses and maintain memory with cytolytic properties, thereby yielding long-term disease control.
In the open-label KEYNOTE-942 trial, patients with adjuvant resected melanoma at high risk of recurrence were randomly assigned 2:1 to receive 1 mg of mRNA-4157 intramuscularly every 3 weeks for up to 9 doses plus 200 mg of pembrolizumab intravenously every 3 weeks for up to 18 cycles (n = 107) or pembrolizumab monotherapy at matched dosing (n = 50).
The trial’s primary end point was RFS. Secondary end points included DMFS and safety. Exploratory end points included assessing ctDNA and BRAF status as potential predictive biomarkers associated with treatment outcomes.
Patients with stage IIIB, IIIC, IIID, or IV cutaneous melanoma that was completely resected within 13 weeks of beginning pembrolizumab therapy were able to enroll on the trial. Additional eligibility criteria included having an ECOG performance status of 0 or 1 and available tissue samples for next-generation sequencing.
Treatment with mRNA-4157 plus pembrolizumab demonstrated improvements in RFS among patients with BRAF mutations (n = 61; HR, 0.332; 95% CI, 0.13-0.85) and those with BRAF wild-type disease (n = 96; HR, 0.808; 95% CI, 0.366-1.784). In a subgroup of patients with BRAF mutations who were ctDNA negative (n = 42), RFS improved with the combination therapy (HR, 0.069; 95% CI, 0.009-0.563). Additionally, Weber reported RFS improvements with the combination among patients with BRAF wild-type disease who were ctDNA negative (n = 68; HR, 0.334; 95% CI, 0.121-0.923).
Of note, any-grade and grade 3 or higher serious adverse effects (SAEs), respectively, affected 14.4% and 12.5% of patients who received mRNA-4157 plus pembrolizumab. The corresponding SAE rates in the single agent pembrolizumab arm were 10.0% and 8.0.
The most common treatment-emergent adverse effects (TEAEs) in the combination and monotherapy arms, respectively, included fatigue (83.7% vs 54.0%), injection-site pain (56.7% vs 2.0%), chills (51.9% vs 6.0%), and pyrexia (51.9% vs 6.0%). Common any-grade immune-mediated AEs in each arm included hypothyroidism (20.2% vs 16.0%), colitis (5.8% vs 4.0%), hyperthyroidism (5.8% vs 6.0%), and pneumonitis (3.8% vs 0.0%).
According to Weber, mRNA-4157 in combination with pembrolizumab will be further assessed in the phase 3 V940-001 study in patients with resected melanoma as well as the phase 3 V940-002 study (NCT06077760) in those with resected non–small cell lung cancer.










