Hurricane Frequency and Other Climate Change Related Events, ‘Disproportionately’ Affects Cancer Care
Climate change is already having major impacts on the cancer patient population.
For some oncology systems in Hurricane Ida’s wake, a dire situation was already made worse by the COVID-19 pandemic.
For Michael J. Castine, MD, a hematologist oncologist with the Hematology Oncology Clinic at Baton Rouge General, a Mayo Clinic Care Network member in Baton Rouge, Louisiana, those effects can be felt firsthand.
“The biggest impact, I think that that we faced from this particular storm, and it was somewhat similar to Katrina 16 years ago was, basically we get an influx of calls in patients that are having a hard time accessing the care where the storm pass through. So, we're just we were just on the edge of that. So, we're catching people who are calling and saying they need their treatments or calling and saying they need help,” said Castine, in an interview with Targeted OncologyTM.
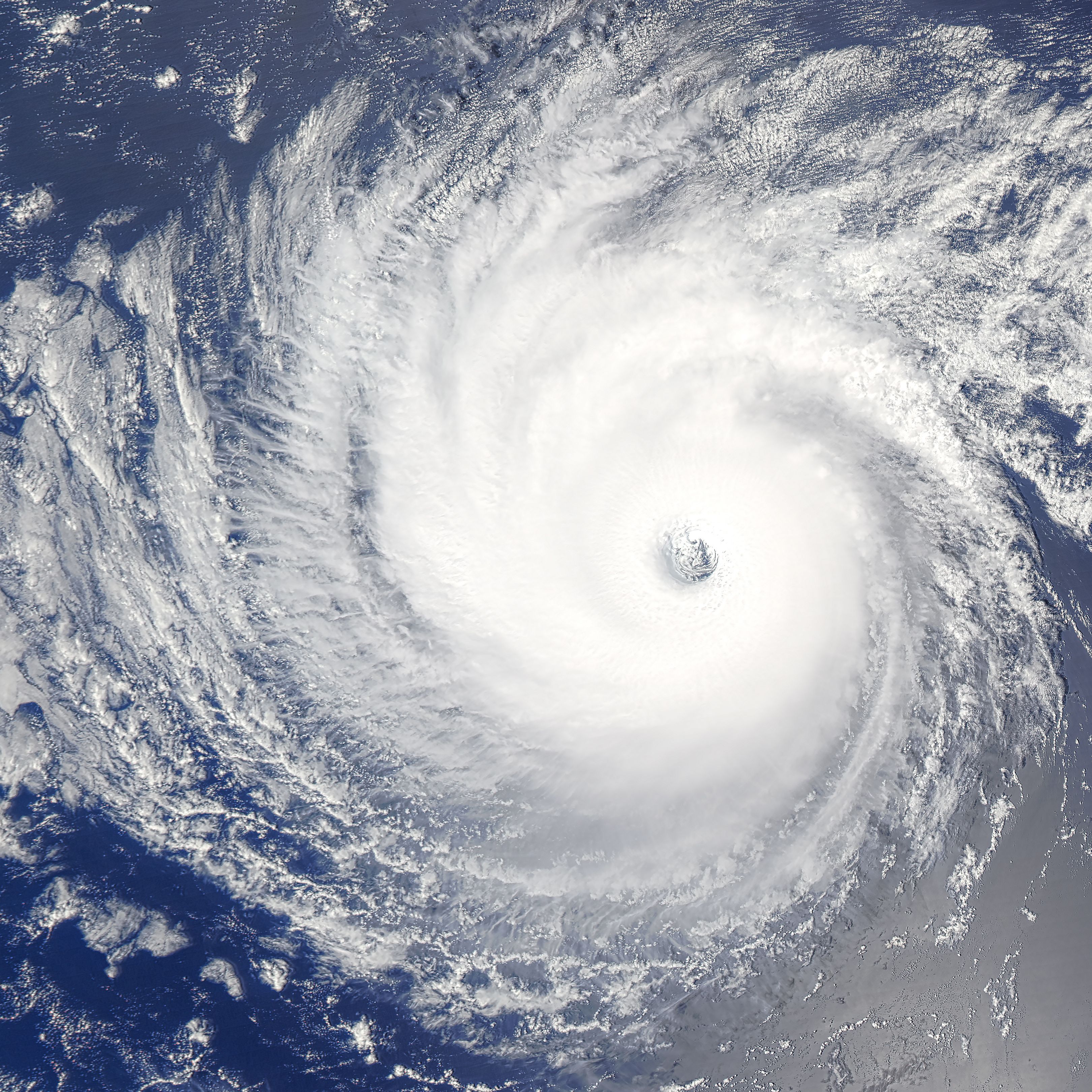
In the United States, Hurricane Ida made landfall at 240 kph (150 miles) near Port Fourchon, Louisiana. Remnants of the storm impacted the mid-Atlantic and Northeast and at least 77 direct fatalities were confirmed, according to a report by insurance provider AON plc. In the United States alone, the damage is estimated to be in the tens of billions.1
Thousands of people were displaced by the storm, any many people receiving cancer care were forced to go elsewhere. For even lightly impacted clinics like Castine’s, the strain was quickly felt.
“Our hospitals are full, because they evacuated all of those people from the nursing homes and from the hospitals and everything out of the path of the storm. And they try to take refuge in places where they think impacts will be less. So, as a consequence, we were already pretty full with COVID. But they're tucking patients in every nook and cranny and every rehab bed and sick bed. And it's made it very difficult for us to conduct normal operations,” said Castine.
According to research, man-made climate change is causing storms like Hurricane Ida to occur at an increased rate and are expected to become more frequent as the Earth continues to warm. A recent study published in Science found that compared to their grandparents born in 1960, the average newborn will experience 3 times as many climate disasters. For example, a person born in 1960 will experience 4 ± 2 heat waves in their lifetime. For a person born in 2020, they will experience 30 ± 9 heat waves during their lifetime if current climate pledges are followed. For tropical storms, the average newborn can experience up to 8 times as many as their grandparents.2
According to Castine, the effects of more frequent storms can be seen across the state. Hurricane Ida hit when there was still lingering damage from other storms.
“The storms are having a definite impact. It's not to say that they can't rebuild, it just takes a long time,” said Castine. “And if you were to drive through Lake Charles right now, I came back through there the day before this storm hit. And they still have blue tarps on roofs [from previous storms] as far as you can see. That's kind of what New Orleans looks like right now.”
The one thing that is clear is that climate change is already having major impacts on the cancer patient population. According to an editorial published in the Journal of Clinical Oncology, the effects of climate change will be disproportionately felt by patients with cancer.3
“These changes will also result in increases in food-borne, water-borne, and vector- borne diseases; an increase in under-nutrition and food insecurity; an increase in incidence and severity of asthma and other respiratory diseases; and an increase in mental health problems,” wrote the authors.3 “These are likely to result in mass migration of climate refugees who are displaced by rising sea levels or economic scarcity, with all of the associated health issues that will befall refugees, and violent conflict resulting from competition among nations for scarcer resources. All of these adverse health effects will be disproportionately worse in our patients with cancer.”
Climate Change Impact on the Cancer Infrastructure
Climate change has had a direct and profound impact on the cancer infrastructure. Disruption to cancer care puts patients at risk, especially since cancer patients tend to need frequent interactions with the health care system. Current patients aren't the only ones at risk. Extreme weather directly impacts screenings and other preventative measures.
Hard data is already available on the correlation between treatment disruption and cancer survivorship. Research published in JAMA Network Open found that patients with lung cancer whose radiotherapy was disrupted by a hurricane had significantly worse outcomes than those who did not experience a treatment disruption.
Investigators matched 1734 patients whose treatment was disrupted to 1734 patients whose treatment was not disrupted by hurricanes between 2004 and 2014. With a median observation time of 15 months, of the 1734 patients who experienced a treatment disruption, there were 1408 reported deaths, a median survival of 29 months, and a 5-year survival estimated of 14.5%. For the 1734 patients who did not experience an interruption, there were 1331 deaths, a mean survival of 31 months, and a 5-year survival estimate of 15.4%. Additionally, patients who experienced a disruption had a median duration of treatment of 66.9 days compared to the 46.2 days of those who did not experience a disruption.4
According to experts with Oncologists United for Climate and Health (OUCH), the severity and frequency of these disruptions will only grow as climate change worsens. This will lead to even bigger impacts than already observed on patient care and wellbeing.
“What we're seeing is that these events are becoming stronger and more frequent. The California wildfire season, for example, is the longest that it's ever been, it's almost all year round now. What used to be one in 100-year storms, for example, a sandy type storm, those are now going to be occurring at a frequency of one in 20 years, right? So, as they become more frequent and more intense, the disruptions get to be more,” said Brian Lestini, MD, PhD, the chief medical officer of a pharmaceutical biotech company and OUCH member.
Climate change is also greatly impacting future patients. During an extreme weather event, routine screenings are often put on hold. Experts predict that as health systems are overrun by a surge in injuries, infections, and communicable diseases causes by extreme weather events, resources will be taken away from preventative programs, like cancer screening, and relocated to disaster response. Increased warming may even affect the accuracy of cancer screening itself.5
A lack of screening has real effects on oncologists treating patients. A lack of screening means cancer is caught in later stages, meaning a decline in the chance of positive outcomes. This theory is supported by what is already being seen with the COVID-19 pandemic.
A report published in Preventative Medicine found that the volume of tests for breast and cervical cancers was well below the previous 5-year averages for the months of March through June of 2020. Within this time span, breast cancer screenings declined 87% from the previous 5-year average. Cervical cancer screenings declined by 84%.6
“With COVID, it is estimated that because of how many patients delayed screening for cancer, that means that there were going to see more patients present with more advanced cancers in the future. And the former head of the National Cancer Institute estimated that there will be about 10,000 excess deaths from colon and breast cancer because of the lack of screening,” said Joan Schiller, MD, adjunct professor at the University of Virginia, board member at the Lung Cancer Research Foundation, and OUCH member, in an interview with Targeted Oncology.
Like with COVID-19, screening disruptions caused by climate change could spell worse outcomes for patients diagnosed with highly treatable cancers such as breast and prostate cancers. Even if the roads and passible and patients are able to make it to the hospital in the aftermath of an extreme weather event, it doesn’t mean they will be able to receive their routine screenings. Radiation oncology services typically cannot be performed on a backup generator. This means that if a hospital is without power, screenings using radiation equipment cannot be performed even if a backup generator is up and running.
The 10-year survival of breast cancer patients was found to be much lower in those who experienced Hurricane Katrina than those who did not. A study published in the Journal of General Internal Medicine looked at 794 patients with breast cancer in parishes affected by Hurricane Katrina. The data sample was matched with 3049 unaffected breast cancer patients. The unadjusted analysis found that Hurricane Katrina was associated with a 15% increase in mortality among breast cancer patients (HR, 1.15; P < 0.05). After adjustments were made for sociodemographic characteristics and cancer stage, Hurricane Katrina was still associated with worse outcomes for this patient population.7
Oncologists and their patients are not the only ones that will be negatively impacted by climate change. The medical supply chain is also highly prone to disruption by climate change. For example, there was a major saline shortage in the wake of Hurricane Maria in 2018. Baxter’s Puerto Rico manufacturing facility, which supplies approximately 50% of United States hospitals with small-volume saline bags, was left without power in the wake of the storm. The other 2 saline manufactures available were not able to make up for the shortage.8 Saline is an essential part of medication delivery. A shortage could cause delays in cancer care.
Patients are not the only ones who need to evacuate during a storm. Hospital staff is also at risk. A review of 85 papers on the impact of natural disasters on cancer care published in The Lancet Oncology found that after an earthquake or tsunami, only 38% to 47% of staff reported to work 1-month after the disaster. Staffing shortages could continue for up to 18 months.9
The same review found that retaining staff in especially prone areas can be very difficult. Damage to facilities often leads to unemployment or workforce displacement. In affected areas, some oncologists reported being unemployed for more than 6 months and many considered early retirement. After Hurricane Katrina, one doctor in training and their coworkers described a 5-year delay in the restoration of an oncology fellowship training program. Ultimately, training was completed in outpatient clinics.9
The loss of paper and electronic medical records is the most common health-care related issue reported by health care systems during natural disasters. The loss of both paper and electronic records was most frequently caused by water damage or collapsed infrastructure. This can create serious problems for often complex oncology treatment regimens. The loss of these documents can complicate follow-up and create difficult future disease management decisions. Health systems should use recoverable electronic medical records in order to safeguard against this issue in the case of a natural disaster.
Damage to health care facilities themselves is also a major problem. The destruction of even part of these facilities can cause major disruptions and the loss of important equipment and records.7
“I was visiting Vanderbilt hospital and went to the radiation oncology department. Nashville had a huge flood… the entire radiation oncology department had flooded with water up to almost the ceiling, because of an intense rain event. All of their linear accelerators, each of which cost about $2 million, they had 3 of those plus their treatment planning machines, all were ruined,” said Christine Berg, MD, OUCH member and National Cancer Institute (retired). “The patients had to go elsewhere for several months to get their treatment. It is a great expense to replace all of the equipment, get it recertified. I met with the lead medical physicists there. And I asked him what Vanderbilt institution was planning for the next time and he goes: sandbags.”
REFERENCES:
1.Global catastrophe recap. Aon. 2021. Accessed October 5, 2021. https://aon.io/3iBYKlX.
2.Thiery W, Lange S, Rogelj J, et al. Intergenerational inequities in exposure to climate extremes. Science. 2021;3740(6564):158-160 doi: 10.1126/science.abi7339
3.Schiller J, Averbuch S, Berg C. Why oncologists should care about climate change. J. Oncol. Prac. 2020; 16(12):775-778. doi: 10.1200/OP.20.00609
4. Association between declared hurricane disasters and survival of patients with lung cancer undergoing radiation treatment. JAMA. 2019;322(3):269-271. doi:10.1001/jama.2019.7657
5.Hiatt R, Beyeler N. Cancer and climate change. Lancet Oncol 2020; 21: e519–27. doi: 10.1016/S1470-2045(20)30448-4
6.DeGroff A, Miller J, Sharma K, et al. COVID-19 impact on screening test volume through the National Breast and Cervical Cancer early detection program, January–June 2020, in the United States. Prev. Med. 2021;151. doi: 10.1016/j.ypmed.2021.106559
7.Bell S, Banerjee M, Griggs J. et al. The effect of exposure to disaster on cancer survival. J GEN INTERN MED 2020;35:80–382. doi: 10.1007/s11606-019-05465-x
8.Mazer-Amirshahi M and Fox E. Saline shortages — many causes, no simple solution. N Engl J Med. 2018; 378:1472-1474 doi: 10.1056/NEJMp1800347
9.Man R, Lack D, Wyatt C, et al. The effect of natural disasters on cancer care: a systematic review. Lancet Oncol. 2018;19(9):E482-E499. doi: 10.1016/S1470-2045(18)30412-1
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.