Fusion Genes Associated With More Aggressive Papillary Thyroid Cancer in Pediatric Patients
The most common genetic cause of alterations in pediatric patients with papillary thyroid cancer were fusion genes, which were associated with more aggressive disease.
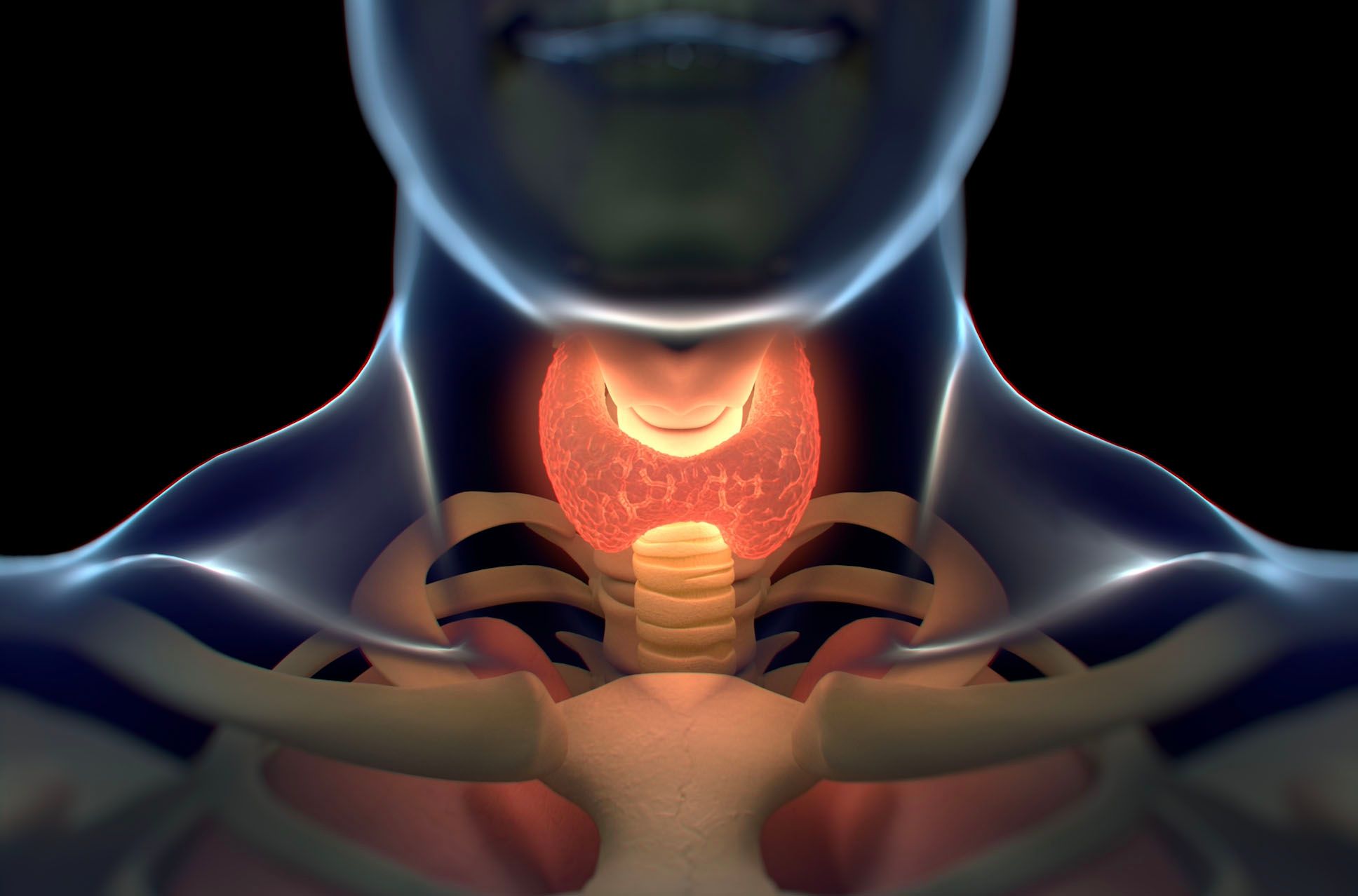
The most common genetic cause of alterations in pediatric patients with papillary thyroid cancer (PTC) were fusion genes, which were associated with more aggressive disease, according to a study published in Thyroid.
In this study, several novel rearrangements were identified, and the fusion genes seemed to be a molecular marker number one in this patient population.
Overall, the study included 93 pediatric patients who had undergone thyroid surgery between 2003 and 2019 at the Department of Ear, Nose, and Throat, Second Faculty Medicine, Charles University, and Motol University Hospital in Prague. The mean age of patients at diagnosis was 14.5 ± 3.4 years, and the female to male ratio was 2.6 to 1. Eighty-two patients had a total thyroidectomy and 11 had a subtotal thyroidectomy, where 10 were completed to total thyroidectomy.
The mean tumor size was 22.1 ± 13.7 mm, and the investigators noted that 17 patients had microcarcinoma. Twenty-six patients (29.9%) had PTC of classical variant, 20 (23.0%) had classical and follicular variant, 29 (33.3%) had follicular variant, 3 (3.4%) had solid variant, 3 (3.4%) had a mixture of classical/follicular/solid variant, 2 (2.3%) had diffuse sclerosing variant, 2 (2.3%) had columnar variant, 1 (1.1%) had tall cell variant, and 1 (1.1%) had case clear cell variant.
After a median follow-up was 72 months (range, 2-198), 11 (19.3%) patients had persistent or recurrent disease at least 1 year after surgery or patients who were in remission and later had a malignant object thyroid tissue formed. Sixteen (19.3%) patients only had biochemical evidence of persistent disease, while 56 (67.5%) remained in remission with no evidence of disease. One patient died due to advanced disease. Additionally, 10 patients were not classified because of short-term follow-up, 84 received radioactive iodine (RAI) treatment, and 8 did not receive RAI because of low-risk disease.
More than half (55.9%) of the patients had fusion genes, which included RET, NTRK1, NTRK3, ALK, BRAF, and MET. Additionally, 10 different types of RET fusions were observed in 26 patients, 4 types of NTRK3fusions in 14 patients, 1 ALK fusion in 6 patients, 2 types of NTRK1 fusions in 3 patients, 2 types of BRAFfusions in 2 patients, and 1 type of MET fusions in 1 patient. Overall, 20 types of fusion genes were identified in the study, 11 of which were interchromosomal and 9 were intrachromosomal rearrangements.
Investigators detected 2 co-existing RET fusions in 1 PTC nodule, which included ACBD5/RET fusion with juxtaposition of exon 11 of the ACBD5 gene and exon 12 of RET gene in the first and BBIP1/RET fusion with a juxtaposition of exon 1 of the BBIP1 gene and exon 8 of the RET gene. CCDC6/RET rearrangement was the most common fusion gene, which was observed in 13 patients (14%), while 1 of these patients had a novel isoform including a part of exon 9 of RET gene. Other rearrangements that were observed more commonly included ETV6/NTRK3 in 10 patients (10.8%), NCOA4/RET, and STRN/ALK both in 6 patients (6.5%) and RBPMS/NTRK3 found in 2 patients (2.2%). The remaining fusions were not recurrent.
BRAF fusions with partner genes, CUL1, and OPTN were reciprocal, and the IRF2BP2/NTRK1 fusion gene has 2 isoforms, 1 being a fusion of exon 1 and the second of exon 2 of the IRF2BP2 gene with exon 10 of the NTRK1 gene. Every isoform was found in a different patient, and no patients with fusion genes had a prior history of radiation exposure before their PTC diagnosis.
The investigators also compared the samples positive for the fusion gene to those that did not harbor this mutation. Positive samples were associated significantly with the mixture of classical and follicular types of PTC (P =.025), and the fusion-positive samples were also significantly associated with extrathyroidal extension (P <.001), higher T classification (P =.009), lymph node metastases (P <.001), distant metastases (P =.021), chronic lymphocytic thyroiditis (P =.001), and frequent occurrence of psammoma bodies (P =.004). Patients who were positive for the fusion gene has also received more frequent multiple doses of RAI therapy (P=.008). Borderline statistically significant associations were observed for features such as tumor size larger in fusion gene-positive tumors (P =.057), number of microcarcinomas higher in fusion gene-negative tumors (P=.052), and a higher number of patients who were not given RAI treatment (P =.058).
Samples that were positive for the fusion genes were different from each other as well, according to the fused oncogene involved. A statistical analysis was only able to be performed between RET and NTRK3 fusion gene-positive samples because of the low number of samples in the other fusion groups. RET fusions were significantly associated with lower mean age of patients at diagnosis (P =.035), lymph node metastases (P =.033), distant metastases (P =.020), and frequent occurrence of psammoma bodies (P =.006). The NTRK3fusions were significantly associated with follicular variant PTC (P =.013).
In RET fusion gene-positive group, 11 patients (42.3%) were of prepubertal age (up to age 12) compared with only 1 patient (7.1%) in the NTRK3 fusion-positive group (P =.021).
All patients with distant metastases (n = 10) had the genetic cause of PTC detected, which was HRAS Q61R point mutation in 1 patient, NCOA4/RET in 4, CCDC6/RET in 2, RASAL2/RET in 1, EML4/MET in 1, and co-occurrence of ACBD5/RET with BBIP1/RET in 1.
Point mutations in BRAF, HRAS, KRAS, NRAS, and TERT genes were assessed in all patients, in which 18 (19%) had the BRAF V600E mutation, and the HRAS Q61R and NRAS Q61K was found in 1 patient each. No mutations were found in the KRAS gene or in the promoter region of TERT. Patients with HRAS-positive PTC (n = 1) underwent radiation treatment for Hodgkin’s lymphoma. The co-occurrence of fusion gene and somatic point alternation was not identified in the study.
These findings demonstrated a point mutation or fusion gene was observed in 72 pediatric patients (77.4%) with PTC, and the oncogenic alteration was unidentified in 21 patients (22.6%). Most tumors were follicular variants of PTC and T1/T2 classification predominated the tumor samples in this study. No patients had experienced recurrence or persistence of structural disease, but 1 patient had biochemical persistence of their disease while almost all of the other patients remained in remission.
Overall, this study demonstrated that fusion genes occurred in 56% of pediatric patients with PTC, and point mutations in the BRAF and RAS genes were observed in 77% of patients. Patients who harbored a fusion gene had more aggressive forms of the disease, which included more frequent extrathyroidal extension, lymph node metastases, distant metastases, and consequently had received more doses of RAI than those without the fusion gene mutations.
Reference
Pekova B, Sykorova V, Dvorakova S, et al. RET, NTRK, ALK, BRAF, and MET fusions in a large cohort of pediatric papillary thyroid carcinomas. Thyroid. Published Online July 1, 2020. doi: 10.1089/thy.2019.0802
Anticipating Novel Options for the RAI-Refractory DTC Armamentarium
May 15th 2023In season 4, episode 6 of Targeted Talks, Warren Swegal, MD, takes a multidisciplinary look at the RAI-refractory differentiated thyroid cancer treatment landscape, including the research behind 2 promising systemic therapy options.
Listen






