FDA’s ODAC Finds Cilta-Cel Favorable in R/R Multiple Myeloma
During an Oncologic Drugs Advisory Committee Meeting, the FDA found that ciltacabtagene autoleucel has a favorable benefit/risk profile in relapsed/refractory multiple myeloma who have received at least 1 prior line of therapy and are refractory to lenalidomide.

- Ciltacabtagene autoleucel (cilta-cel; Carvykti) is a chimeric antigen receptor T-cell (CAR-T) therapy approved by the FDA in February 2022 for patients with multiple myeloma who have already undergone multiple prior treatment lines.
- The FDA’s Oncologic Drugs Advisory Committee (ODAC) has voted that the benefits of ciltacabtagene autoleucel (cilta-cel; Carvykti) do outweigh the risks for this indication.
- The discussion during the meeting focused on the overall survival (OS) data from the CARTITUDE-4 study (NCT04181827).
The FDA’s ODAC determined the risk/benefit assessment for cilta-cel for the treatment of adult patients with relapsed or refractory multiple myeloma, who have received at least 1 prior line of therapy, including a proteasome inhibitor (PI), and an immunomodulatory agent (IMID), and are refractory to lenalidomide to be favorable.1
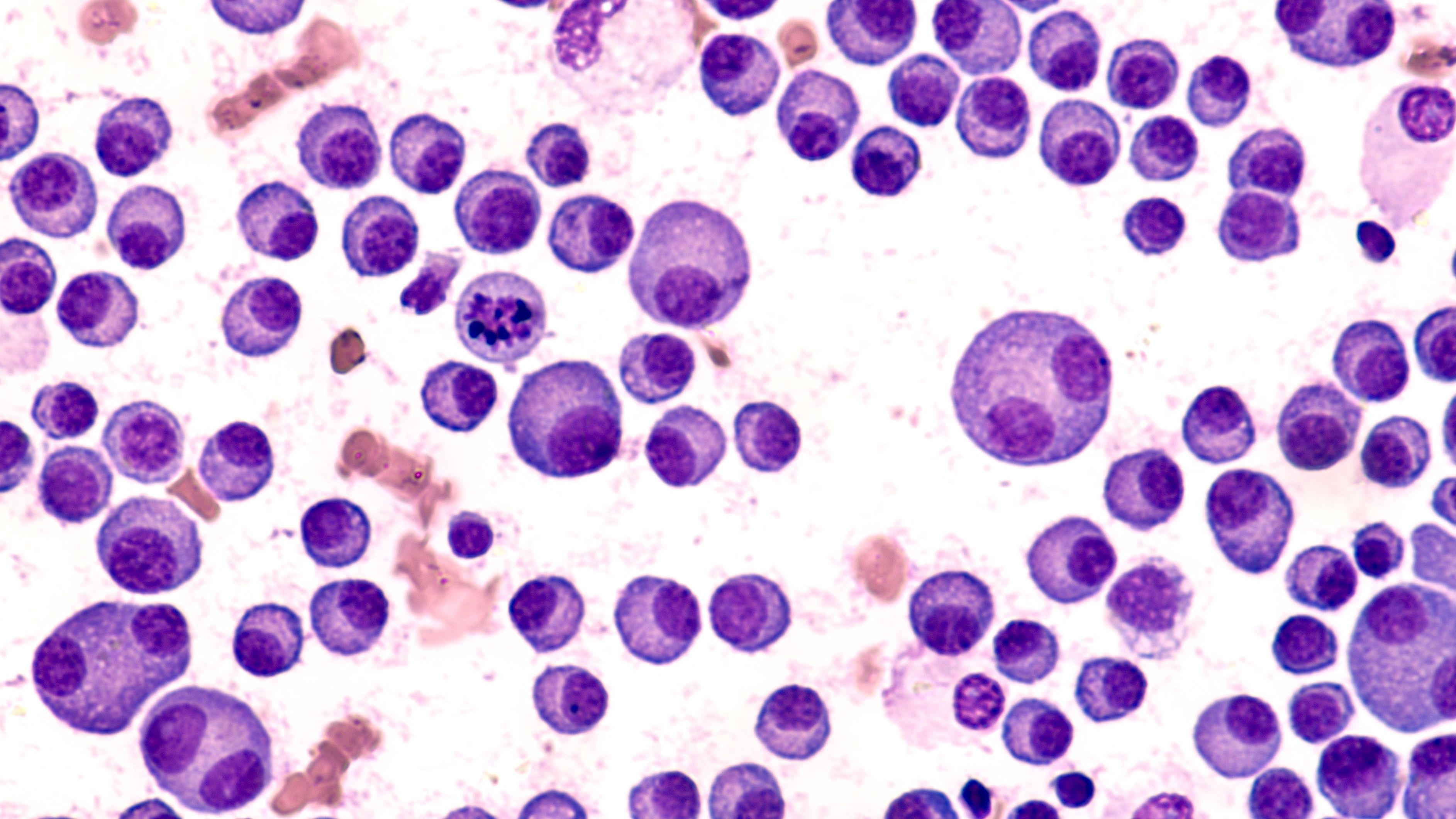
Bone marrow aspirate cytology of multiple myeloma: ©David A Litman - stock.adobe.com
The discussion from the Committee focused on the overall survival (OS) data in the CARTITUDE-4 study and the risks and benefits of cilta-cel in the intended population.
“The review issues are that cilta-cel led to a significantly improved rate of progression-free survival, but with a decrement in overall survival in the first 10 months of the trial. The decrement in overall survival calls into question whether the risk/benefit assessment is favorable,” said Rob Sokolic, chief, malignant hematology branch, Office of Clinical Evaluation, Office of Therapeutic Products, Center for Biologics Evaluation and Research, FDA.
Discussion questions for the meeting included:
- Do the results of CARTITUDE-4 are sufficient to support a positive risk-benefit assessment of cilta-cel for the approved indications?
- Is the risk of early death associated with cilta-cel acceptable in the context of PFS benefit?
About the Phase 3 CARTITUDE-4 Trial
CARTITUDE-4 is a randomized, open-label, phase 3 trial which included patients with lenalidomide-refractory multiple myeloma.2 Patients were treated with either cilta-cel or the physician’s choice of effective standard care. All the patients included (n = 419) in the study had received 1 to 3 prior lines of treatment, and 208 received cilta-cel and 211 received 1 of 2 standard-of-care regimens, either pomalidomide, bortezomib, and dexamethasone (PVd) or daratumumab (Darzalex), pomalidomide, and dexamethasone (DPd).
The primary end point evaluated in the study was progression-free survival (PFS) as determined by a blinded independent review committee using the International Myeloma Working 2016 criteria. OS is a key secondary end point in CARTITUDE-4, along with stringent complete response (sCR), complete response (CR), minimal residual disease (MRD) negativity, and overall response rate (ORR).
At a median follow-up of 15.9 months (range, 0.1-27.3), the median PFS was not reached (95% CI, 22.8-not evaluable [NE]) among those given cilta-cel vs 11.8 months (95% CI, 9.7-13.8) among those given the standard of care (HR, 0.26; 95% CI, 0.18-0.38; P <.001). At 12 months, the PFS rate was 75.9% (95% CI, 69.4%-81.1%) for those given cilta-cel vs 48.6% (95% CI, 41.5%-55.3%) among those given the standard of care.
In the cilta-cel group vs standard-of-care group, 84.6% and 67.3% had an overall response, 73.1% and 21.8% had a CR or better, and 60.6% and 15.6% had an absence of MRD. OS data continues to strengthen as the data mature.
“We saw cilta-cel significantly reduced the risk of disease progression or death vs standard of care by 74%. Cilta-cel led to significantly higher rates of response and default response compared with standard of care,” explained Binod Dhakal, MD, MS, assistant professor of medicine in the Division of Hematology and Oncology at the Medical College of Wisconsin, in an interview with Targeted OncologyTM. “These results suggest cilta-cel is highly effective and provides superior efficacy responses compared with standard-of-care in the study.”
“The beneficial results were consistently observed across every subgroup that we assessed,” Jordan Schecter, MD, vice president, research and development, Johnson & Johnson Innovative Medicine, explained during the meeting.
Regarding safety, 39 patients and 46 patients across arms died, respectively, (HR, 0.78; 95% CI, 0.5-1.2), and the majority of patients had a grade 3 or 4 adverse event during treatment. In the as-treated population, which included 176 patients treated with cilta-cel, 134 (76.1%) had cytokine release syndrome (CRS), 1.1% of which was grade 3 or 4. No grade 5 CRS was seen. Also in this group, 8 (4.5%) patients had immune effector cell-associated neurotoxicity syndrome, all of which were grade 1 or 2, 1 had movement and neurocognitive symptoms deemed grade 1, 16 (9.1%) had cranial nerve palsy (grade 2, 8.0%; grade 3, 1.1%), and 5 (2.8%) had peripheral neuropathy that was related to CAR T-cell therapy (grade 1 or 2, 2.3%; grade 3, 0.6%).
“The safety profile of cilta-cel in the CARTITUDE-4 study is consistent with its known safety profile in the approved label and is consistent with the mechanism of action of CAR T cells,” Sen Zhuang, MD, PhD, vice president, oncology research and development, Johnson & Johnson, said during the meeting.
CAR T-cell therapy in multiple myeloma: © Kasloom - stock.adobe.com
Applicant Stance
Cilta-cel gained FDA approval in February 2022 based on data from the phase 1b/2 CARTITUDE-1 study (NCT03548207).3,4 In CARTITUDE-1, patients received cilta-cel via a single infusion at a dose range of 0.5 to 1.0 x 106 CAR-positive viable T cells per kg of body weight.2
In the study, the ORR was 98% (95% CI, 92.7%-99.7%), and the sCR rate was 78% (95% CI, 68.8%-86.1%). At a median follow-up of 18 months, the median duration of response was 21.8 months (95% CI, 21.8-NE). With extended follow-up, the median PFS was 33.9 months (95% CI, 25.5-NE). This compared with the historical control of approximately 3 to 5 months.1
The median time to first response was 1 month with a median time to CR or better of 2 months (range, 1-15).2,3 A total of 57 patients were evaluated for MRD, and 91.8% were MRD-negative. At 18 months, the PFS rate was 66.0% (95% CI, 54.9%-75.0%) and the OS rate was 80.9% (95% CI, 71.4%-87.6%). Among patients with sustained MRD for more than 6 months and more than 12 months, the PFS rate was 96.3% and the OS rate was 100%. The median PFS was not reached.
For safety, grade 3/4 hematologic AEs included neutropenia (94.8%), anemia (68.0%), leukopenia (60.8%), thrombocytopenia (59.8%), and lymphopenia (49.5%). CRS was reported in 94.8% of patients but was predominantly grade 1 and 2.
On June 6, 2023, Janssen Biotech, Inc., submitted a supplemental biologics licensing application (sBLA) for cilta-cel, seeking approval for the agent as a treatment of adult patients with relapsed/refractory multiple myeloma who have received at least 1 prior line of therapy, including a PI and an IMID and are refractory to lenalidomide, at a dose range of 0.5‑1.0×106 CAR-positive viable T cells per kilogram of body weight to a maximum dose of 1×108 CAR-positive viable T cells per single-dose infusion.1
To further evaluate cilta-cel for this indication, the applicant discussed the CARTITUDE-4 trial. According to Zhuang, cilta-cel led to clinically meaningful, highly statistically significant PFS rates vs the standard-of-care combinations.
“These deep and durable responses are nonobtainable by the standard treatment modalities and with additional follow-up, translated into a strong trend and improvement of overall survival that has further strengthened this,” explained Zhuang. “Additionally, subgroup analyses demonstrate consistent benefit of cilta-cel in both progression-free survival and overall survival across all subgroups.”
Irene Ghobrial, MD, professor of medicine, Dana-Farber Cancer Institute, Harvard Medical School, went on to explain the unmet needs for patients with lenalidomide-refractory multiple myeloma as they often have poor outcomes with standard therapy.
“There remains a significant and critical unmet need for new therapeutic options in the patients to be used,” said Ghobrial.
With the use of earlier CAR T-cell therapy, patients are offered the chance at deeper remissions, better long-term outcomes, and a 1-time infusion which will help the CAR T-cell benefits for patients. Additionally, the use of CAR T-cell therapy earlier also links with less ongoing exposure to the therapy.
Sundar Jagannath, MD, director of center of excellence for multiple myeloma, Tisch Cancer Institute, professor of medicine at Icahn School of Medicine Mount Sinai, then joined the conversation to discuss the “outstanding” clinical efficacy observed with cilta-cel in CARTITUDE-4. He first noted the clinically meaningful PFS improvement, followed by the trend toward improved OS. Additionally, he noted that the MRD negativity rate of 88% in evaluable patients support the potential for improved long-term outcomes.
“Data were consistent across all of the subgroups. The data do not support the exclusion of any specific patients, and all patients have the potential to experience meaningful benefit from cilta-cel,” explained Jagannath during the meeting.
Specifically, Jagannath explained that while patients who have relapsed after 1 to 3 prior lines of therapy now have several FDA-approved triplet regimens available to them, these options have largely been tested in patients who are lenalidomide-naive, showing that lenalidomide treatment often leads to patients becoming lenalidomide-refractory. The median PFS among patients who have lenalidomide-refractory multiple myeloma is < 12 months, and regimens that are based on continuous therapy until progression often have cumulative toxicity and significant treatment burden.
“Of course, we must consider the safety…There are risks with cilta-cel, as with any therapy; however, the risk is well understood by physicians and is manageable,” added Jagannath.
Specifically, CRS and immune effector cell-associated neurotoxicity syndrome were observed in the trial, but most were mild and able to be resolved with standard CAR T-cell management. Additional neurotoxicity events were mild. For infections observed, COVID-19 was prevalent. Now, the risk has been minimized through less prevalence of serious COVID, vaccinations, and further understanding of the disease.
Through insights from Jagannath, Ghobrial, Zhuang, and more, the applicant believes that cilta-cel provides a significant clinical benefit for this patient population and would be a key option for patients with multiple myeloma who are lenalidomide-refractory.
FDA Perspective
The main topic for discussion brought up by the FDA was the increased rate of early death observed among patients treated with cilta-cel in CARTITUDE-4. The CARTITUDE-4 trial showed cilta-cel to be effective in improving PFS for patients with multiple myeloma compared with standard therapy. However, there was a higher rate of early deaths in the cilta-cel arm.
As a result, the FDA determined that further discussion is needed regarding the adequacy of exploratory analyses from the CARTITUDE-4 trial. Ideally, these analyses would help identify strategies to mitigate the risk of early deaths associated with cilta-cel.
“The results show a lower overall survival in the cilta-cel arm compared to the standard therapy arm that appears to extend to 10 months with the curves crossing after that,” explained Helkha Peredo-Pinto, MD, MPH, medical officer, clinical reviewer, malignant hematology branch, Division of Clinical Evaluation Hematology, Office of Clinical Evaluation, Office of Therapeutic Products, CBER, during the meeting. “The crossing pattern of the Kaplan-Meier curves for overall survival renders the average hazard ratio not interpretable.”
The FDA typically recommends OS serves as the primary end point in oncology trials and is considered the "gold standard" because it is not biased, directly addresses extending life, and captures the treatment's safety impact by reflecting all causes of death.
In addition to OS, in which Peredo-Pinto explained that early OS detriment was seen in the cilta-cel arm with a pattern of crossing of the curves, she discussed PFS. She explained that while there was a statistically significant improvement in median PFS seen with cilta-cel vs standard therapy, the median PFS was not reached in the cilta-cel arm vs 12 months for the standard therapy. With these results, a higher proportion of PFS events led to death in the cilta-cel arm vs the standard of care arm.
“There were 17 deaths in the cilta-cel arm vs only 4 deaths in the standard therapy arm,” explained Peredo-Pinto.
The FDA generally approves drugs with a statistically significant and clinically meaningful benefit on PFS, along with an acceptable risk profile. The higher early death rate in the cilta-cel arm raises questions about whether the overall benefit-risk assessment is favorable for cilta-cel.
“The study was not designed to identify predictive factors for early mortality observed with cilta-cel. The higher rate of early death appears to be an inherent risk of autologous CAR T-cell therapy. Overall, there is an uncertain benefit/risk of cilta-cel in the proposed population,” added Peredo-Pinto.
As a result, the FDA believes that more data might be necessary to definitively assess the benefit/risk profile of cilta-cel. This could involve further analysis of the CARTITUDE-4 data or results from ongoing trials.
ODAC’s Decision
The FDA’s ODAC ultimately decided that the risk of early death associated with cilta-cel was acceptable in the context of PFS benefit and that the results of CARTITUDE-4 are sufficient to support a positive risk/benefit assessment for the proposed indication.
“Cilta-cel brings significant clinical benefit compared with other approved therapies based on improved efficacy and has changed the treatment landscape for late-stage patient care. Being able to provide these deep and durable responses and the chance for improved progression-free survival and overall survival to patients with lenalidomide-refractory multiple myeloma would be invaluable,” explained Jagannath.