FDA Approves sBLA for Reduced Teclistamab Dose in R/R Multiple Myeloma
The reduced dosing frequency of 1.5 mg/kg every 2 weeks for teclistamab in relapsed/refractory multiple myeloma who have sustained a complete response or better for at least 6 months provides flexibility in dosing schedules for patients.

- The FDA approved the reduced dosing frequency of 1.5 mg/kg every 2 weeks for teclistamab-cqyv (Tecvayli) in patients with relapsed/refractory multiple myeloma who have sustained a complete response (CR) or better for at least 6 months.
- Results from the phase 1/2 MajesTEC-1 study (NCT03145181; NCT04557098) supported this approval.
- The reduced dosing frequency demonstrated promising efficacy outcomes, with an overall response rate (ORR) of 63.0% and a CR rate or better of 39.4%.
A supplemental biologics license application (sBLA) for teclistamab to be administered at a reduced dose of 1.5 mg/kg every 2 weeks has been approved by the FDA for the treatment of patients with relapsed/refractory multiple myeloma who have achieved and maintained a CR or greater for at least 6 months, according to Johnson & Johnson, the agent’s manufacturer.1
"[Teclistamab] is the only BCMA-targeted immune-based therapy with weight-based dosing. [This] approval of biweekly dosing for eligible patients will further enable clinicians to meet the individual needs of patients who may want flexibility in their dosing schedules," said Rachel Kobos, MD, vice president, Oncology Research & Development, Johnson & Johnson Innovative Medicine, in a press release.
Results from the phase 1/2 MajesTEC-1 study supported the agency’s decision. In the single-arm, open-label, multicohort, multicenter dose-escalation study, patients were given the recommended phase 2 dose (RP2D) of teclistamab at 1.5 mg/kg weekly given subcutaneously, and those who had a confirmed CR or better for at least 6 months were then eligible for the reduced dose frequency which continued until disease progression or unacceptable toxicity. At a median follow-up of 14.1 months, the reduced dosing frequency yielded an ORR of 63.0% and a 39.4% CR rate or better.2
Further, 26.7% of patients had no minimal residual disease (MRD), and the MRD-negativity rate among patients who had a CR or better was 46%. Median duration of response was 18.4 months (95% CI, 14.9-not estimable), while median progression-free survival was 11.3 months (95% CI, 8.8-17.1).
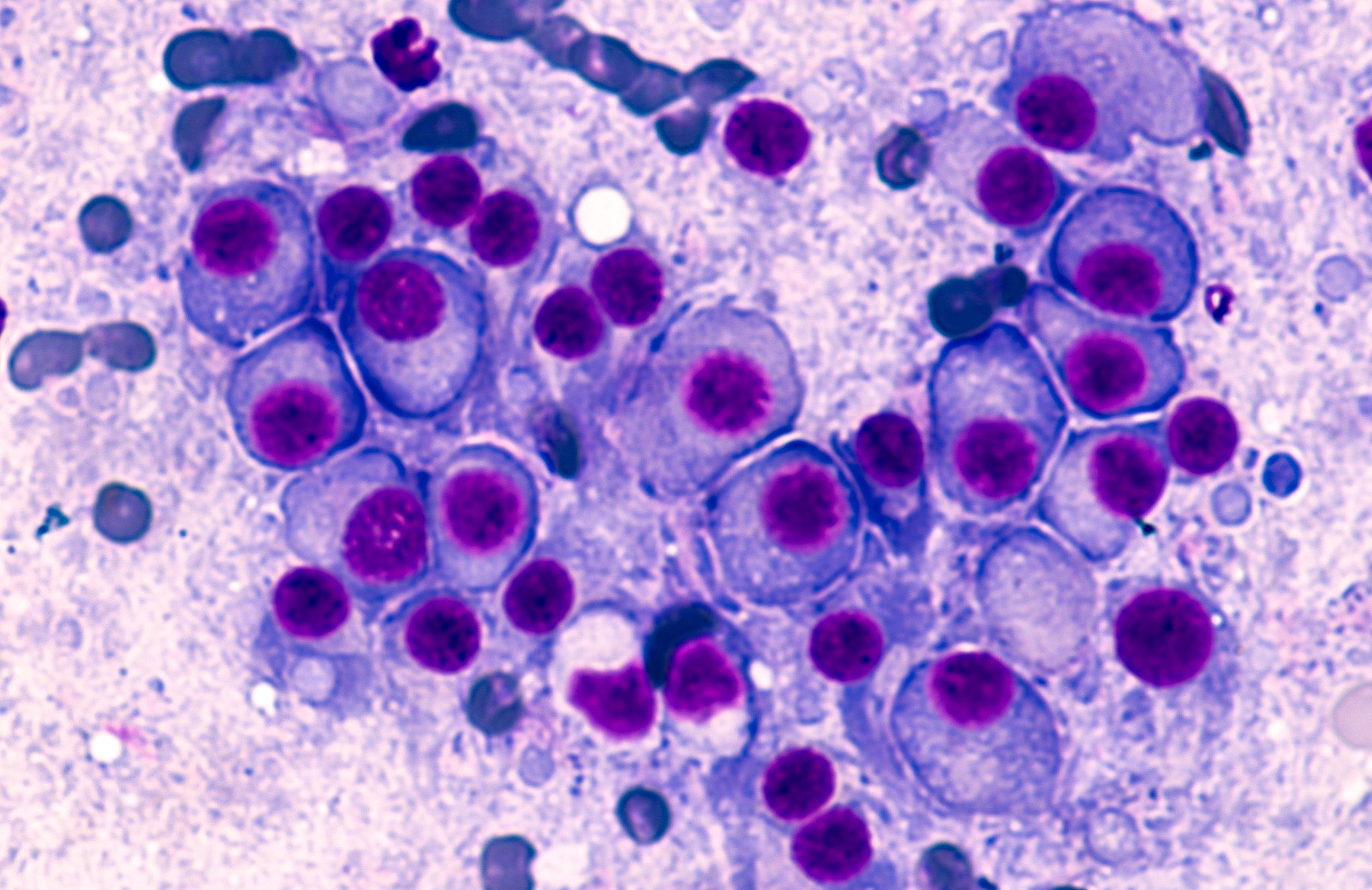
Multiple Myeloma: © David A Litman - stock.adobe.com
Looking at safety, the most common any-grade adverse effects (AEs) observed among those treated with teclicstamab were cytokine release syndrome (CRS; 72.1%), neutropenia (70.9%), anemia (52.1%), and thrombocytopenia (40.0%). These AEs were grade 3/4 in 0.6%, 64.2%, 37.0%, and 21.2%, respectively. Neurotoxic events were seen in 14.5% of patients and included grade 1/2 immune effector cell-associated neurotoxicity syndrome in 5 patients.
In October 2022, the FDA granted accelerated approval to teclistamab for the treatment of adult patients with relapsed/refractory multiple myeloma. This indication is for those who have received at least 4 prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody.
MajesTEC-1 Study Background
MajesTEC-1 sought to evaluate the efficacy and safety of teclistamab in 165 adult patients with relapsed/refractory multiple myeloma who received at least 3 prior lines of therapy.including an immunomodulatory drug, a proteasome inhibitor, and an anti-CD38 antibody.3
The phase 1 portion of the trial included a dose-escalation portion and a dose expansion component to explore the safety, tolerability, pharmacokinetics, and preliminary efficacy of teclistamab in this patient population. In the phase 2 portion of the trial, investigators evaluated the efficacy of teclistamab at the RP2D of subcutaneous 1.5 mg/kg weekly. Patients were offered to switch to receive a dose every other week if they achieved at least a partial response to treatment after 4 or more cycles of therapy in phase 1 or at least a CR for 6 or more months in phase 2.
The primary end point of this study was ORR, which was assessed with the International Myeloma Working Group (IMWG) 2016 criteria. The Common Terminology Criteria for Adverse Events (CTCAE) version 4.03 were used to grade AEs, whereas the American Society for Transplantation and Cellular Therapy guidelines were used for immune effector cell-associated neurotoxicity syndrome and CRS.
References
(Teclistamab-cqyv) biweekly dosing approved by the U.S. FDA for the treatment of patients with relapsed or refractory multiple myeloma. News release. Johnson & Johnson. February 20, 2024. Accessed February 21, 2024. http://tinyurl.com/yc8h6k63
Moreau P, Garfall AL, van de Donk, N WCJ. Teclistamab in relapsed or refractory multiple myeloma. N Eng J Med. 2022;387(6):495-505. doi:10.1056/NEJMoa2203478
Dose escalation study of teclistamab, a humanized BCMA*CD3 bispecific antibody, in participants with relapsed or refractory multiple myeloma (MajesTEC-1). ClinicalTrials.gov. January 3, 2024. Accessed February 21, 2024. https://classic.clinicaltrials.gov/ct2/show/NCT03145181
Gasparetto Explains Rationale for Quadruplet Front Line in Transplant-Ineligible Myeloma
February 22nd 2025In a Community Case Forum in partnership with the North Carolina Oncology Association, Cristina Gasparetto, MD, discussed the CEPHEUS, IMROZ, and BENEFIT trials of treatment for transplant-ineligible newly diagnosed multiple myeloma.
Read More