Experts Reflect on Most Impactful FDA Moves of 2020 in Solid Tumors, Hematologic Malignancies
Experts in oncology and hematology review some of the most impactful FDA approvals from 2020 in lung, breast, blood, gastrointestinal, and genitourinary cancers.
Despite the rapid spread of the coronavirus disease 2019 (COVID-19) that plagued not only the oncology field but the healthcare system as a whole, the treatment options for patients with countless different solid tumors and hematologic malignancies were expanded with a number of new FDA approvals indicated throughout 2020. These approvals cover updates in lung, breast, gastrointestinal (GI), and genitourinary (GU) cancers, as well as a variety of hematologic malignancies and other solid tumors.
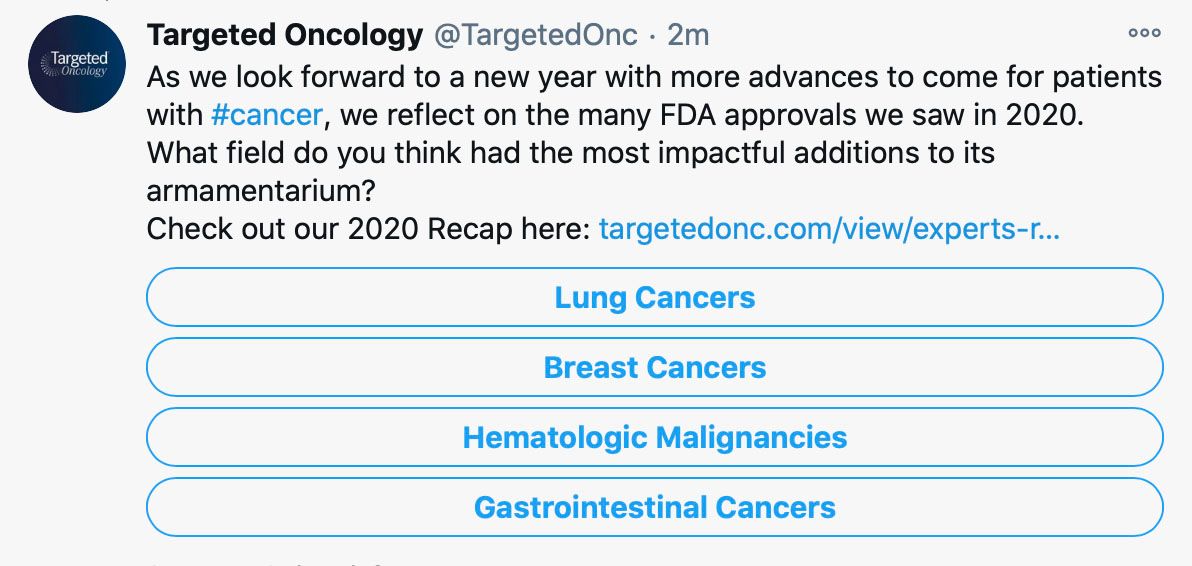
On Twitter, Targeted Oncology asks in a poll, “In what field do you think had the most impactful additions to its armamentarium?” The options include lung cancer, breast cancer, hematologic malignancies, and gastrointestinal cancers.
As the year comes to a close, the FDA continues to advance the field with more approvals coming through. On Friday, December 18, 2020, alone, the FDA granted 5 indications approval. These include ponatinib (Iclusig) for treatment of adult patients withs chronic-phase chronic myeloid leukemia who have become resistant or intolerant to therapy following at least 2 prior tyrosine kinase inhibitors (TKIs), osimertinib (Tagrisso) as adjuvant treatment of patients with non–small cell lung cancer (NSCLC) whose tumors harbor an EGFR exon 19 deletion or exon 21 L858R mutation for use following tumor resection, the triplet regimen selinexor (Xpovio) plus bortezomib (Velcade) and dexamethasone for the treatment of adult patients with multiple myeloma who have received at least 1 prior therapy, oral relugolix (Relumina) for the treatment of advanced prostate cancer, and a biosimilar to rituximab (Rituxan) was approved for the treatment of adult patients with non-Hodgkin lymphoma (NHL), chronic lymphocytic leukemia (CLL), granulomatosis with polyangiitis, and microscopic polyangiitis.
These approvals follow many others that have provided hope throughout the year to physicians and healthcare providers across the United States, but 1 striking area of advancements worth noting this year is the recently approved Emergency Use Authorizations for 2 separate vaccinations for the prevention of coronavirus disease 2019 (COVID-19), which plagued the world, particularly impacting oncology practices treating immunocompromised, sick patients. These approvals, including the BNT162b2 vaccination and the mRNA-1273 Moderna COVID-19 Vaccine on December 18, 2020, demonstrate a crucial step in overcoming the pandemic.
Mark Lewis, MD

“We've learned this year what we can do quickly without being overly hasty, and I think COVID-19 was the ultimate impetus for unity,” Mark Lewis, MD, director, GI Oncology, Intermountain Healthcare, told Targeted Oncology. “At my center, which is not primarily a research institution, we've run almost 40 trials around COVID-19, largely in-patient, but also largely driven by the clinical need and queries of our intensivists, among others. It's shown us that given the right prompt, you can actually move pretty fast, and learn things very quickly.”
Despite the challenges brought on by the pandemic, the healthcare system remained dedicated to keeping patients with cancer safe. Telehealth played a major role in this, as well as other adjustments physicians and cancer centers have made in light of this pandemic. These changes are not only keeping patients safe during these unprecedented times, but they lay the groundwork for the future of treating these patients better in the community setting.
“I think we've learned what has to be done at a major research institution and what can be done either at a [community] center or even in the patient's home,” said Lewis. “Oncology, for a long time, unfortunately, has not been very patient-centric. The idea has been, you're sick, but you need to come to us. Obviously, there are still patients that absolutely have to make that effort to come see us, but on the flipside, we've learned what we can you do remotely and what we can do to bring treatment and research to the patient rather than the other way around.”
One important update in the field of oncology in light of the COVID-19 pandemic was the FDA’s approval of a new dosage for pembrolizumab (Keytruda) in April 2020, reducing the frequency of clinic visits for patients with cancer. The prior dosage for this immune checkpoint inhibitor was 200 mg every 3 weeks, which remains an approved dosing option, but the newly approved dose of 400 mg is administered every 6 weeks, which is approved across all indications whether the PD-1 inhibitor is given as a monotherapy or in a combination regimen. Pembrolizumab is approved across many disease types and has also gained tumor agnostic approvals over the last few years as well.
“We have these really sweeping histology agnostic approvals, and I think the biggest 1 that comes to mind for me is the FDA setting eligibility for immune therapy at a tumor mutational burden [TMB] of greater than 10 mutations/megabase. I think that was pretty amazing,” said Lewis. “Just in the last couple years, we've seen this shift towards histology agnosticism, whether it's about NTRK fusion proteins, which have become a unicorn in oncology that every oncologist looks for, or we're talking about microsatellite instability [MSI]-high status and eligibility for pembrolizumab.”
The immune checkpoint inhibitor pembrolizumab received approval in June 2020, for use in adult and pediatric patients with unresectable or metastatic solid tumors with tissue TMB–high who have progressed on prior therapy and have no satisfactory alternative treatment options. This marks the second tumor-agnostic approval for the agent, following a prior approval from 2017, for the treatment of patients with MSI–high or mismatch repair deficient solid tumors.
“While we have these very broad indications, now we're also seeing every cancer become a rare cancer. One thing I've seen [more of] this year is selecting out molecular subsets of disease, and a great example is the approval of pralsetinib [formerly BLU-667; Gavreto] for RET-positive tumors, whether of the lung or the thyroid,” Lewis said. “I think we're seeing that across the categories, which is just site of origin largely, and you can see these mutations that might occur in both lung and thyroid, for the example of RET, and presumably be targetable with the same agent.”
Lung Cancer
Pralsetinib (Gavreto) gained approval in September 2020 for the treatment of RET fusion-positive NSCLC based on findings from the phase 1/2 ARROW study (NCT03037385), and a few short months later, the RET inhibitor also received approval for use in patients with advanced or metastatic RET-mutant medullary thyroid cancer, as well as those with RET fusion-positive thyroid cancer, also supported by the ARROW data.
Similarly, selpercatinib (formerly LOXO-292; Retevmo) capsules, was approved the treatment of patients with either lung or thyroid cancer who harbor RET alterations. This therapy received approval in May 2020, marking it the first approved treatment to target RET. Specifically, the indications for selpercatinib include adult patients with metastatic RET fusion–positive NSCLC, adult and pediatric patients 12 years of age and older with advanced or metastatic RET-mutant medullary thyroid cancer who require systemic therapy, or patients with advanced or metastatic RET fusion-positive thyroid cancer who require systemic therapy and who are radioactive iodine (RAI)–refractory, if RAI was appropriate.
Several new therapies gained approval in lung cancer in 2020 across a variety of subsets. In particular, capmatinib (Tabrecta) was approved in May 2020, for the treatment of patients with metastatic NSCLC whose tumors have a MET exon 14 skipping mutation based on the findings from the phase 2 GEOMETRY mono-I study (NCT02414139). This approval fills a gap in the landscape for patients with NSCLC since no other approved therapies target the MET exon 14 mutation in advanced disease.
In March 2020, the FDA approved durvalumab (Imfinzi) as a frontline treatment for adult patients with extensive-stage small cell lung cancer (ES-SCLC) in combination with standard-of-care chemotherapy, etoposide and carboplatin, or cisplatin, offering a new therapeutic approach to a population of patients who have had limited treatment options up until recently. The approval was based on findings from the phase 3 CASPIAN study (NCT03043872), which showed overall survival (OS) analyses favored the durvalumab arm across patient subgroups compared with chemotherapy alone.
Breast Cancer
The field of breast cancer saw a number of new advances during the year of 2020, many of which impacting patients with metastatic and advanced disease. The FDA granted approval across a number of subsets of patients, including those with HER2-positive disease, triple-negative breast cancer (TNBC), and hormone receptor (HR)-positive disease.
William J. Gradishar, MD

“In each of these areas, in the very recent past, there's been a marked expansion of therapeutic options,” William J. Gradishar, MD, chief of hematology and oncology, department of medicine, Betsy Bramsen Professorship of Breast Oncology, professor of medicine (hematology and oncology), Northwestern University's Feinberg School of Medicine, told Targeted Oncology. “We still have a lot of work to do, patients are still dying of metastatic breast cancer, but we've made significant progress in not only preventing recurrences from developing in patients with early-stage disease, but we've also extended the survival of patients who have metastatic disease.”
The FDA granted approval in February 2020 to neratinib (Nerlynx) in combination with capecitabine for the treatment of adult patients with advanced or metastatic HER2-positive breast cancer who received at least 2 prior anti-HER2-based regimens in the metastatic setting. This approval was based on supportive findings from the phase 3 NALA trial (NCT01808573). This study showed a 24% reduction in the risk of disease progression or death compared with lapatinib (Tykerb) and capecitabine. Prior to this, neratinib was approved for use as extended adjuvant treatment in adult patients with early-stage HER2-positive disease following adjuvant trastuzumab-based therapy.
In combination with trastuzumab (Herceptin) and capecitabine, tucatinib (Tukysa) received FDA approval for the treatment of adult patients with advanced unresectable or metastatic HER2-positive breast cancer in April 2020, including patients with brain metastases who have received at least 1 prior line of HER2-based therapy in the metastatic setting. This approval sparked a lot of excitement in the field, receiving its indication from the FDA 4 months ahead of the Prescription Drug User Fee Act (PDUFA) target action date. The oral, small molecule TKI of HER2 received its approval based on the phase 2 HER2CLIMB study (NCT02614794), which showed a 46% reduction in the risk of disease progression or death among heavily pretreated patients with unresectable, locally advanced, or metastatic HER2-positive disease.
“An abundance of new drugs in the HER2 space is a great thing because we can go from 1 therapy to the next. For patients with advanced disease, tucatinib and neratinib are examples of that; these all expand the number of options we have for patients, and tucatinib in particular shows clear evidence of activity in the brain, which is critically important,” Gradishar said. “In the triple-negative space, sacituzumab govitecan [Trodelvy] is an example of an antibody-drug conjugate [ADC] that has activity, and then, of course, the approval of pembrolizumab has expanded the number of treatment options we have for patients with triple-negative disease.”
In April 2020, sacituzumab govitecan received accelerated approval for the treatment of adult patients with metastatic TNBC who have received at least 2 prior lines of therapy for metastatic disease, based on the findings from the phase 3 ASCENT study (NCT02574455). The study demonstrated that sacituzumab govitecan, the first ADC approved specifically in mTNBC, had induced an objective response rate (ORR) of 33.3% (95% CI, 24.6%-43.1%), and the clinical benefit rate was 45.4%, which included stable disease for at least 6 months.
The immune checkpoint inhibitor pembrolizumab plus chemotherapy was approved for the treatment of patients with locally recurrent unresectable or metastatic TNBC whose tumors express PD-L1, and this news was joined by approval of the PD-L1 Immunohistochemistry (IHC) 22C3 pharmDx as a companion diagnostic for identifying patients likely to derive benefit from this therapy. The FDA granted this approval based on the findings from the phase 3 KEYNOTE-355 clinical trial (NCT02819518), which showed statistically significant and clinically meaningful improvement in the median progression-free survival (PFS) of 9.7 months with pembrolizumab and chemotherapy compared with 5.6 months in the chemotherapy-alone arm (HR, 0.65; 95% CI, 0.49-0.86; one-sided P =.0012).
Among other updates in breast cancer, the combination of pertuzumab, trastuzumab, and hyaluronidase-zzxf (Phesgo) by subcutaneous injection was approved by the FDA in June 2020 for the treatment of patients with HER2-positive breast cancer that has spread to other parts of the body, as well as for the treatment of adult patients with early HER2-positive breast cancer. This approval, which came 4 months ahead of the PDUFA date, is the first regimen approved for subcutaneous administration that contains 2 monoclonal antibodies. In the FeDeriCa study (NCT03493854), Phesgo was found to have comparable efficacy and safety to the intravenous regimen of pertuzumab and trastuzumab, meeting the study’s primary end point of non-inferiority.
Hematologic Malignancies
Naveen Pemmaraju, MD

“There have been a lot of fantastic FDA approvals in the hematologic malignancy space, and obviously, we have to think about multiple myeloma,” said Naveen Pemmaraju, MD, associate professor, Department of Leukemia, Division of Cancer Medicine, The University of Texas MD Anderson Cancer Center, in an interview with Targeted Oncology. “When I started out as a faculty 10 years ago, there were just not that many drugs approved, and so in the multiple myeloma space now as a consequence of 5 to 10 years of clinical trials, many of which were negative, we are seeing the appearance of some of these drugs.”
Multiple myeloma saw approval of a number of new indications throughout 2020, including the May 2020 approval of daratumumab in combination with hyaluronidase-fihj (Darzalex Faspro) as treatment of adult patients with newly diagnosed or relapsed/refractory multiple myeloma, allowing a subcutaneous dosing of daratumumab. The regimen is approved under several indications for patients with multiple myeloma based on findings from the phase 3 COLUMBIA (NCT03277105) and the PLEIADES (NCT03412565) clinical trials. This approval offers patients a more convenient therapeutic option as the fixed-dose injection is administered in approximately 3 to 5 minutes, considerably reducing the treatment burden for these patients.
The immunoconjugate targeting B-cell maturation antigen (BCMA) belantamab mafodotin-blmf (GSK2857916; Blenrep) gained approval in August 2020, for the treatment of patients with relapsed/refractory multiple myeloma who previously received at least 4 prior lines of therapy, which should include an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 antibody. This is the first anti-BCMA therapy available for these patients anywhere in the world, which was supported by a unanimous vote from the FDA’s Oncologic Drugs Advisory Committee. Based on findings from the phase 2 DREAMM 2 clinical trial (NCT03525678) exploring 2.5-mg/kg and 3.4-mg/kg doses, the lower dose received the FDA’s recommendation as an intravenous infusion given over approximately 30 minutes once every 3 weeks.
Selinexor, the only nuclear export inhibitor approved by the FDA for use in 2 hematologic malignancies, generated excitement in the field. This includes the triplet regimen of selinexor with bortezomib/dexamethasone in multiple myeloma that gained approval in December 2020, as well as the accelerated approval for single-agent treatment with selinexor in adult patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) not otherwise specified, who have had at least 2 prior systemic therapies, including patients with DLBCL arising from follicular lymphoma. This marks the only single-agent oral therapy approved for patients with relapsed/refractory DLBCL.
Andrew M. Evens, DO, MSc

“We saw a lot of movement in the DLBCL space. Up until before CAR T was approved, frankly, we had almost nothing besides chemotherapy. Now in the span of a year, we not only have CAR T-cell therapy, but we have a couple of other agents including tafasitamab which is in combination with lenalidomide and is an active antibody against CD19,” Andrew M. Evens, DO, MSc, of the Rutgers Cancer Institute of New Jersey, told Targeted Oncology. “Selinexor is the other FDA-approved agent that is an option for patients, so it’s promising to me in a very difficult disease, especially when relapsed/refractory, just to have now a multitude of agents approved.”
The combination of tafasitamab-cxix (Monjuvi) with lenalidomide (Revlimid) was approved for the treatment of adult patients with relapsed/refractory DLBCL not otherwise specified, including disease arising from low-grade lymphoma and patients who are not eligible for autologous stem cell transplant. The accelerated approval was granted on the basis of findings from the phase 2 L-MIND study (NCT02399085) on the safety and efficacy, as well as the observational retrospective cohort RE-MIND study (NCT04150328) on the real-world use of tafasitamab, the CD19-directed monoclonal antibody.
Alexey V. Danilov, MD, PhD

“The approval of tafasitamab and lenalidomide came up this year, and that was certainly a very exciting approval. It is a very innovative chemotherapy-free approach to treatment of patients with relapsed/refractory DLBCL,” Alexey V. Danilov, MD, PhD, associate professor of medicine at the Oregon Health & Science University, said to Targeted Oncology. “CAR T-cell therapy in mantle cell lymphoma [MCL] has been approved this year as well, and that is also life changing for patients with MCL, where we've had very limited options in those who progressed on ibrutinib or ibrutinib and venetoclax. That's a life-changing option.”
The autologous CD19-directed CAR T-cell therapy brexucabtagene autoleucel (formerly KTE-X19; Tecartus) received FDA approval for the treatment of adult patients with relapsed or refractory MCL in July 2020, based on findings from the phase 2 ZUMA-2 clinical trial (NCT02601313). According to Evens, the ORR among the first 60 patients treated and followed for at least 7 months was 93% (95% CI, 84%-98%), and the overall ORR was 85%. The 1-year PFS rate was 61%, and the estimated 1-year OS rate was 83%. Findings demonstrated cytokine release syndrome was observed in 91% of patients with 15% being grade 3 or higher in severity and none being fatal. Neurologic events, another notable side effect associated with CAR T-cell therapy, were observed in 63% with 31% being grade ≥3 and none being fatal.
GI Cancers
“Not every patient needs next-generation sequencing, but there are some cancer types where you can make a strong argument that is becoming almost mandatory,” said Lewis. “A great example from this also would be biliary tract cancers. With cholangiocarcinoma and gallbladder cancer, we know that they are underneath the umbrella groups of highly targetable mutations, whether it's IDH1 or FGFR2. Now, thankfully, it's not just an academic exercise to find the mutation because now we have a drug to pair with it, so another FDA approval I would call attention to was pemigatinib [Pemazyre] for FGFR2-driven cholangiocarcinoma because when I started, there was literally 1 drug for biliary tract cancer, gemcitabine, and now slightly over a decade later, there are a host of possibilities.”
Pemigatinib received approval in April 2020, for the treatment of adult patients with previously treated, unresectable locally advanced or metastatic cholangiocarcinoma who harbor an FGFR2 fusion or rearrangement, representing the first approved treatment for this indication. Findings from cohort A of the phase 3 FIGHT-202 study (NCT02924376) supported this approval, demonstrating an ORR of 36% and a median duration of response of 9.1 months in the multicenter, open-label single-arm study.
The combination of atezolizumab (Tecentriq) plus bevacizumab (Avastin) was approved as treatment of patients with unresectable or metastatic hepatocellular carcinoma (HCC) who have not had a prior systemic therapy, based on findings from the phase 3 IMbrave150 study (NCT03434379). This study demonstrated a reduced risk of death by 42% with the combination compared with sorafenib (Nexavar) alone (HR, 0.58; 95% CI, 0.42-0.79; P =.0006). Compared with standard of care sorafenib, this regimen is the first to markedly improve survival in the frontline setting for patients with HCC in several years.
In addition, the treatment landscape for patients with HCC was enriched with an approval in March 2020 of nivolumab (Opdivo) in combination with ipilimumab (Yervoy) in patients who have been previously treated with sorafenib. This approval allows for a new second-line option for patients with advanced HCC that has demonstrated promising improvements in OS, according to findings from the phase 1/2 CheckMate-040 study (NCT01658878). This study showed the longest duration of OS in the second-line setting for advanced HCC tested in clinical trials.
Patients with colorectal cancer (CRC) also saw a couple of new additions to the armamentarium, with 1 notable approval being the combination of encorafenib (Braftovi) and cetuximab (Erbitux) as treatment for patients with metastatic CRC with a BRAF V600E mutation, as detected by an FDA-approved test, after prior therapy. The combination received its approval from the FDA based on findings from the phase 3 BEACON CRC study (NCT02928224), which showed significant improvements in OS and a higher response rate compared with standard treatment. Shortly after this news, the FDA granted approval to the therascreen BRAF V600E Kit (therascreen® BRAF V600E RGQ PCR Kit) as a companion diagnostic for this regimen.
GU Cancers
In the field of GU cancers, the FDA granted several approvals in 2020, providing more treatment options and hope for physicians treating patients with various diseases. In particular, several approvals in prostate cancer stood out, as well as the first and only approval of an immunotherapy that has demonstrated significant overall survival (OS) benefit in the frontline setting in a phase 3 study of bladder cancer; the FDA granted approval to frontline maintenance avelumab (Bavencio) as treatment of patients with locally advanced or metastatic urothelial carcinoma who have not progressed with frontline platinum-based chemotherapy. Avelumab maintenance extended the OS by 50% compared with best supportive care in the phase 3 JAVELIN Bladder 100 study (NCT02603432).
Petros Grivas, MD, PhD

“Overall, in my opinion, this is practice-changing because right now instead of finishing chemotherapy frontline and waiting until progression happens, we can utilize avalumab based on this study as a switch maintenance frontline approach,” Petros Grivas, MD, PhD, 1 of the principal investigators in the JAVELIN Bladder 100 trial, told Targeted Oncology.
The study demonstrated a 7.1-month improvement in the median OS with frontline avelumab maintenance and best supportive care versus best supportive care alone. The median OS was 21.4 months with avelumab (95% CI, 19.9-26.1) versus 14.3 months in the control arm (95% CI, 12.9-17.9), which was a statistically significant improvement with a 31% reduction in the risk of death in the overall population (HR, 0.69; 95% CI, 0.56-0.86; 2-sided P = .001).
In prostate cancer, the approval of 2 PARP inhibitors excited the field. In May 2020, the FDA approved olaparib (Lynparza) for the treatment of patients with metastatic castration-resistant prostate cancer(mCRPC) who have deleterious or suspected deleterious germline or somatic homologous recombination repair (HRR) gene mutations and have progressed following prior therapy with a new hormonal agent. The approval of this PARP inhibitor was based on findings from the phase 3 PROfound clinical trial, which demonstrated a 66% reduction in the risk of disease progression or death with olaparib versus enzalutamide (Xtandi) or abiraterone acetate (Zytiga) in patients with BRCA1/2 or ATM mutations.
A few days prior to this approval, rucaparib (Rubraca) received FDA approval for adult patients with mCRPC who have a deleterious BRCA mutation (germline and/or somatic)-associated disease and have received prior androgen receptor-directed therapy and a taxane-based chemotherapy. The TRITON trials provided supportive data for this approval, exploring the use of rucaparib in patients with mCRPC and alterations in HRR-related genes.
Maha Hussain, MD

“Olaparib was approved in prostate cancer, and rucaparib also, so around summertime, there were 2 approvals issued by the FDA. The companion diagnostic was also approved for testing for the patients,” said Maha Hussain, MD, who is the Genevieve E. Teuton Professor of Medicine in the Division of Hematology and Oncology, Department of Medicine, and deputy director at the Robert H. Lurie Comprehensive Cancer Center of the Northwestern University Feinberg School of Medicine, in an interview with Targeted Oncology. “What I'm looking forward to is more approvals from the FDA in prostate cancer. I have to say in my career time, the last 10 years have been really tremendous in terms of the approvals from the FDA in the castration-resistant space. It's exciting times. We've been set back by COVID-19, but I do think that we are on a move forward and an upward ladder, so to speak, in terms of better research, and looking forward to much better times and 2021 and onwards.”
The FoundationOne®Liquid CDx approval was expanded as a companion diagnostic for olaparib in November 2020. The test was initially granted approval in August 2020 for the indication of patients with any solid tumor. This olaparib indication followed news from October 2020, indicating FoundationOne CDx as a companion diagnostic to identify patients who may receive benefit from rucaparib, alectinib (Alecensa), or alpelisib (Piqray), which are approved in different solid tumors. In the prostate cancer space, the companion diagnostic is used to identify BRCA1/2 and ATM genes in patients with mCRPC who are eligible for treatment with olaparib.
“There is a lot of excitement about PARP inhibitors, and there are many PARP inhibitors right now that are undergoing evaluation in prostate cancer, which is exciting,” said Hussain. “The research in prostate cancer has really blossomed in an incredible way at multiple fronts, and so I do think we're seeing acceleration in terms of the research and its outcomes.”