Evolving Treatment Paradigms with Amivantamab in Wild-Type NSCLC
Natasha Leighl, MD, MMSc, BSc, discussed the analysis of the CHRYSALIS study that was presented at the 2024 American Association for Cancer Research Annual Meeting.
Natasha Leighl, MD, MMSc, BSc

While amivantamab (Rybrevant) is an established treatment option for patients with non-small cell lung cancer (NSCLC) and was recently approved in EGFR exon 20 insertion-mutated NSCLC, its usefulness in wild-type NSCLC still is under investigation.
Findings from the phase 1b CHRYSALIS study (NCT02609776) investigated the effectiveness and safety of amivantamab in patients with wild-type NSCLC whose disease worsened after standard therapy with platinum-based chemotherapy and anti-PD(L)1 agents. Patients with adenocarcinoma and squamous cell carcinoma were included.
In patients with adenocarcinoma, the overall response rate was 7%, with a 29% chance of some disease control. Responses were short-lived, lasting an average of 4.2 months. However, patients without KRAS or HER2 alterations appeared to benefit more, with a 20% response rate compared with 0% in patients with those alterations.
In patients with squamous cell carcinoma, the response rate was 21%, and some patients experienced responses lasting over 6 months. The disease control rate was 43%, and the median time to disease progression was 4 months.
According to Natasha Leighl, MD, MMSc, BSc, lead of medical oncology at Princess Margaret Cancer Centre in Toronto, Ontario, Canada, and professor of medicine at the University of Toronto, amivantamab showed initial effectiveness in treating patients with wild-type NSCLC, and the regimen warrants further exploration.
In an interview with Targeted OncologyTM, Leighl discussed the analysis of the CHRYSALIS study that was presented at the 2024 American Association for Cancer Research Annual Meeting.
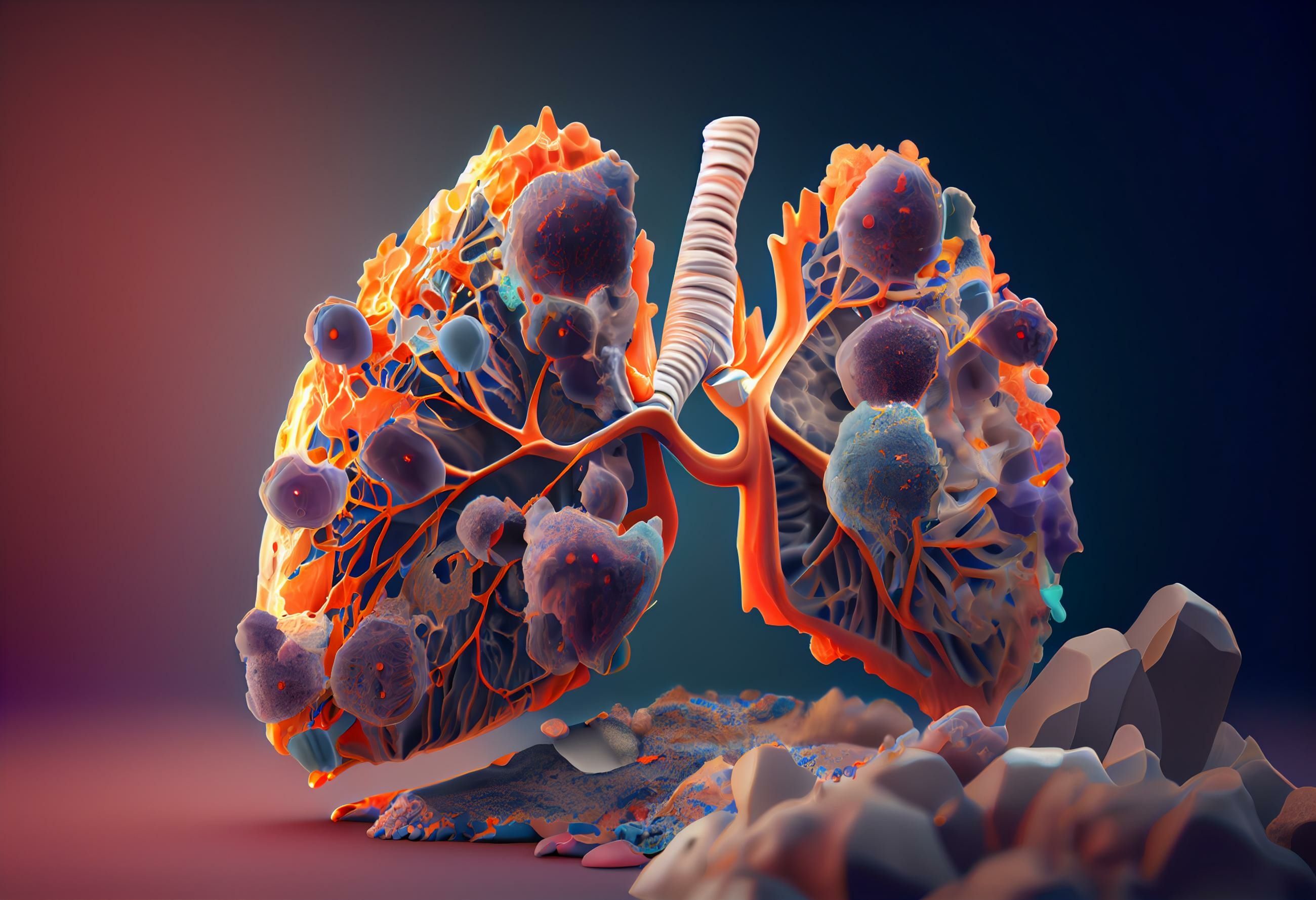
KRAS G12C mutation in non-small cell lung cancer: © Aiden - stock.adobe.com
Targeted Oncology: What is the current treatment landscape of wild-type advanced non-small cell lung cancer?
Leighl: After patients with wild-type non-small cell lung cancer have received chemo-immunotherapy or immunotherapy followed by chemotherapy, the outlook is pretty bleak. Currently, we have docetaxel as the next line of treatment. But there really are not a lot of good options for these patients, and it is a clear unmet need to improve current outcomes.
What are some of the challenges that this disease state presents in particular compared with other types of non-small cell lung cancer?
We've had so much success with targeted therapy, minimal toxicity, great outcomes. And even with immunotherapy with checkpoint inhibition, we have about 20% of patients who have these extraordinary outcomes, they're in response for years with minimal side effects. But for many of our other patients who don't derive these benefits, chemotherapy still remains an important part of treatment, chemo-immunotherapy to start and more chemotherapy after that. It really is a challenge to find that next great breakthrough for these patients. There's very little to guide us molecularly or even immunologically in terms of how to improve their outcomes.
How has amivantamab been used so far?
Amivantamab is a very exciting drug. It's a bispecific antibody that targets both EGFR and MET and also has some immune self-directing activity. It's currently approved for patients with EGFR exon 20 insertion mutant lung cancer, both as subsequent therapy after platinum-based chemotherapy and used on its own, and also more recently in combination with platinum chemotherapy plus amivantamab in the first-line setting for patients with EGFR exon 20 insertion mutant disease. We've also seen a lot of exciting combination data for patients with the more common sensitizing EGFR mutations with the addition of lazertinib, both in pretreated patients as part of CHRYSALIS and more recently in the MARIPOSA study in the first-line setting.
What were the goals of the study presented at AACR?
The CHRYSALIS study was the first study that our team participated in with amivantamab. This really looked at exploring the activity of amivantamab either as monotherapy or in combination with specific therapies in different groups. In particular, this led to approval of amivantamab in those with EGFR exon 20 insertion mutations and also a lot of excitement in patients with MET-driven tumors and other EGFR-driven tumors. We also looked at patients with wild-type lung adenocarcinoma and also wild-type squamous carcinoma as well to see whether this concept of using targeting with a bispecific antibody for EGFR and MET,which is also important in wild-type tumors and would lead to disease improvement.
Could you summarize your findings?
In the 2 cohorts, we were able to look at 41 patients with wild-type lung adenocarcinoma and 14 patients with wild-type squamous carcinoma. We found that the safety profile in these groups was very similar to what we'd seen with amivantamab. Patients’ toxicities were mostly EGFR- and MET-mediated. We saw some early mild infusion reactions, but usually teams can overcome this quite early, and they don't tend to recur.
What was very interesting to us was the activity. The overall response rate in patients with adenocarcinoma was 7%. The disease control rate was higher, at about 29%. The immediate duration of response was just over 4 months. But using plasma [circulating tumor DNA (ctDNA)] or liquid biopsies, we were able to look at patients based on genotyping. We found that if patients had KRAS or HER2 alterations in their tumor, they were unlikely to have a response or benefit. But if they didn't have KRAS alterations, and we know that those are often not seen in patients with EGFR alterations, or they didn't have HER2 alterations, the response rate went up to 20% in that group, so the potential to exclude some patients for EGFR, that may not be as important and to really increase that response rate to 20%. So that was quite exciting. It's a small study with a small number of patients, but certainly higher than the historical response rate for docetaxel.
We also saw very similar and unexpected findings in patients with wild-type squamous lung cancer. The response rate was 21%. In this group, again, a small group of patients, but the median duration of response has not yet been reached, and at least 2 patients have been in response for more than 6 months now. So again, very, very exciting, and a median [progression-free survival] of four months. This is a group of patients that historically does badly. But we know that EGFR expression is common in patients with squamous lung cancer. And so again, this concept of targeting the EGFR protein with the bispecific antibody on the cell, and does this lead to sustained benefits for patients? Based on these, we think that these are very exciting early results.
We saw antitumor activity in patients with refractory wild-type adenocarcinoma or squamous cell carcinoma. In fact, in the patients with squamous cell disease, none of our patients have yet progressed. And in particular, in those with adenocarcinoma, we were able to really refine the group of patients that benefited by identifying those without KRAS or HER2 alterations in tumors.
What are the implications of these findings?
There's a lot of excitement looking at [antibody drug conjugates (ADCs)], which, of course, have a lot of toxicity, or combinations [with ADCs]. With these early findings, 1 of the questions arises, can we use amivantamab in these wild-type tumors? Is this better than checkpoint inhibition with chemotherapy in patients with low or negative PD-L1 [expression]? We don't know. But is that important, especially in patients with squamous lung cancer? Or could we add this to other treatments like docetaxel and improve outcomes, perhaps with less toxicity than with ADCs? And finally, can we learn more about how to select these patients? Maybe EGFR protein expression is important in these squamous wild type patients. And clearly this exclusion of patients with KRAS and HER2 alterations is also very important in patients with wild-type adenocarcinoma. Are we able to use some of these things, perhaps to even identify a group that might benefit from this minimally toxic monotherapy? I think there's a lot of potential promise ahead, both with the combination, moving into earlier lines of treatment and improving our molecular selection [of] patients.
What are the next steps from these findings?
I think that based on the key takeaways that we have, so far, we've seen antitumor activity; we're learning more about where it works. Now, I think we need to look at the landscape and see where the gaps are. And I think, in particular, with patients with squamous lung cancer, this is a group that does very poorly and so could we use this instead of docetaxel? Could we move this up in the treatment landscape, add it to chemotherapy? Will that improve patient outcomes? And then similarly, for our wild-type adenocarcinoma patients,can we incorporate this into current treatment protocols so that we can actually further improve outcomes? Again, adding minimal toxicity, for example, compared [with] ADCs?