Evolving Paradigms in Soft Tissue Sarcoma: Current Treatment Strategies
This section covers the Current Treatment Strategies section of the current Evolving Paradigms in Soft Tissue Sarcoma issue.
Current Treatment Strategies
Surgery
First-line treatment for STS is surgical resection of the tumor, as well as the surrounding normal tissue, to achieve negative margins.8,11In the event of positive margins, surgery can be performed again to remove additional tissue as long as tissue function is not compromised.8Zagars et al found that local control rates were better among patients who underwent re-resection, with rates of 85%, 85%, and 82% at 5, 10, and 15 years, respectively.21Local control rates were lower among patients who did not undergo re-resection, with rates of 78%, 73%, and 73%, respectively (P= .03). In rare cases of extremity STS, amputation may be necessary but is avoided whenever possible.8,11
Radiotherapy
Radiotherapy and chemotherapy may be used as additional treatment strategies, especially for high-grade, deep, or >5 cm tumors.8,11These treatment approaches can be used together or independently, before surgery to shrink the tumor, and/or after surgery to kill remaining cancer cells. Per guidelines, radiotherapy dose should be administered with best technique to total 50 Gy in 1.8 to 2 Gy fractions.11Radiation techniques include external beam radiation therapy (EBRT), brachytherapy, and proton beam radiation.
The most common radiation technique is EBRT.8During EBRT, radiation dose is administered as high-energy x-rays from outside the body. Intensity modulated radiation therapy (IMRT) is a form of EBRT, but is adjusted to be more specific to the tumor size and shape. This specification reduces the radiation dose to healthy tissue.22In a comparison of conventional EBRT with IMRT, Folkert et al evaluated 319 patients with surgically resected, extremity STS and found that IMRT reduced the risk for local recurrence compared with EBRT.23Patients who received IMRT were older and were more likely to have received preoperative radiation and to have positive margins and higher tumor grade.
Intraoperative radiation therapy (IORT), another form of EBRT, is administered during surgery after the tumor is removed but before the wound is closed and is usually followed by another radiotherapy technique.8This technique reduces the radiation dose to healthy tissue. In a phase II study, Roeder et al found that 5-year rates of local control, distant control, and OS were 97%, 66%, and 79%, respectively, with the combination of IORT and EBRT.24They concluded that these results compared favorably with previous studies that reported local control rates of 80% to 90%.
Brachytherapy, when radioactive material is placed in the tumor bed, can be dosed at a high-dose rate or low-dose rate.8High-dose radiation is administered in a short time period, while low-dose radiation is administered over several days. Compared with IMRT (median dose 63 Gy), brachytherapy (median dose 45 Gy) had worse local control rates.25Patients receiving IMRT tended to have worse features, such as larger tumors and positive surgical margins. Proton beam radiation uses protons to deliver radiation instead of photons.26This reduces radiation dose to normal tissue. Availability of proton beam radiation therapy is limited and so is the evidence supporting its use.8
The timing and dose intensity of radiation can affect clinical outcomes.8,11Although timing of radiotherapy does not affect survival outcomes and local control, complications differ between preoperative and postoperative dosing. Preoperative dosing is associated with wound complications, and postoperative dosing is associated with long-term side effects, such as fibrosis and joint stiffness.27,28
According to retrospective studies, boosts of postoperative radiation after preoperative radiotherapy do not improve local control and increase the risk of long-term complications compared with preoperative radiotherapy alone.29,30High-dose therapy, 60 Gy or 66 Gy, is also associated with increased risk of long-term complications.31Holt et al retrospectively evaluated 364 patients with lower extremity STS and found that higher-dose therapy was associated with more bone fractures than lower-dose therapy, at 50 Gy (P= .007).
First-Line Chemotherapy
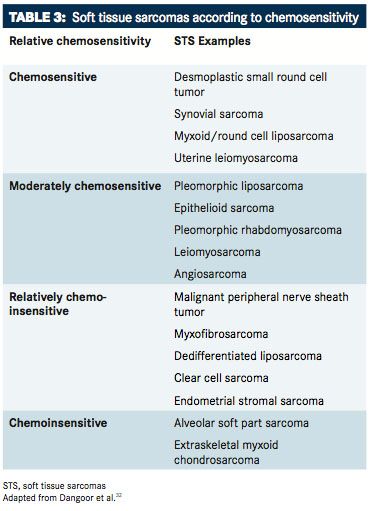
The benefit of chemotherapy for the treatment of localized STS is unclear, but chemotherapy is typically used when metastases are present in advanced disease.8,11In a meta-analysis, Pervaiz et al determined that doxorubicin with ifosfamide in patients with localized STS provided marginal benefits, with an absolute risk reduction in death of 11%.33
However, Woll et al found no added benefit with adjuvant chemotherapy.34In this phase III study, they randomized 351 patients with stage II-III STS without metastases to receive adjuvant chemotherapy of doxorubicin with ifosfamide or no chemotherapy.34Relapse-free survival and OS were similar between groups. However, the ifosfamide dose evaluated, 5 g/m2, was lower than the 9 g/m2 dose evaluated by Frustaci et al, who concluded that adjuvant chemotherapy improved survival.35,36Also, 24% of patients had tumors <5 cm, which are usually not treated with chemotherapy. Woll et al found a slight benefit with adjuvant chemotherapy in an updated meta-analysis (HR 0.86; 95% CI, 0.76-0.97;P= .02).34
Benefits of chemotherapy are more apparent in high-grade, high-risk disease. In a cohort-based analysis, Italiano et al found that adjuvant chemotherapy was significantly associated with improved 5-year metastasis-free survival and OS in patients with grade 3 disease but not in patients with grade 2 STS.37In a comparison of historical matched-control patients and 48 patients treated with doxorubicin, ifosfamide, and dacarbazine, improvements in rates of OS were observed with neoadjuvant chemotherapy in patients with high-grade STS (45% vs 79%, respectively;P= .003).38
An anthracycline-based regimen is standard first-line chemotherapy for advanced STS, specifically doxorubicin.8,11Doxorubicin may also be combined with ifosfamide, but there is no overwhelming evidence supporting combination therapy over monotherapy. In a meta-analysis of randomized controlled trials, combination therapy with doxorubicin and ifosfamide was associated with higher tumor response rates, but survival outcomes were similar to doxorubicin alone.39In addition, adverse events (AEs) were worse with combination therapy. In cases where tumor response is especially advantageous, combination therapy may be preferred.11
As with standard combination therapy, dose-intensified combination therapy does not improve OS. In a phase III trial, Judson et al randomly assigned 455 patients with advanced STS to receive doxorubicin 75 mg/m2 or doxorubicin 75 mg/m2 and 25 mg/m2 with ifosfamide.40Dose-intensified combination therapy was associated with better progression free survival (PFS; 7.4 vs 4.6 months, respectively) and overall response compared with doxorubicin alone, but it did not improve OS. It was also associated with greater rates of AEs, especially leucopenia, febrile neutropenia, anemia, and thrombocytopenia. The authors suggested dose-intensified combination therapy when the treatment goal is tumor shrinkage.40
Second-Line Chemotherapy
Second-line chemotherapies for STS include ifosfamide alone, gemcitabine with or without docetaxel, and dacarbazine with or without gemcitabine, although evidence of efficacy is limited.11As a second-line therapy, ifosfamide is administered to patients who have not previously progressed on ifosfamide or is administered at a higher dose in patients who previously received a standard dose. Gemcitabine has demonstrated efficacy in angiosarcoma and leiomyosarcoma as a single agent, although combination therapy may be more effective. In a phase II trial, Maki et al randomized 122 patients with STS to receive gemcitabine alone or with docetaxel and found that PFS and OS were better with combination therapy than monotherapy (PFS at 6.2 vs 3 months; OS at 17.9 vs 11.5 months, respectively), although toxicity was greater.41Pautier et al, however, found similar survival outcomes between single-agent and combination therapy in a phase II study evaluating patients with leiomyosarcomas, specifically.42
The combination of dacarbazine with gemcitabine also improves survival outcomes compared with dacarbazine alone.43,44In a phase II study, Garcia del Muro et al randomly assigned 113 patients with advanced STS to receive dacarbazine alone or with gemcitabine.43OS was 16.8 months with combination therapy and 8.2 months with monotherapy (P= .014). PFS and objective response rates (ORRs) were also significantly different in favor of combination therapy. A systematic review performed by Sharma et al also demonstrated improved PFS with combination therapy.44The 3-month PFS rate was 54.2% with combination therapy and 35.2% with monotherapy.
Trabectedin, originally derived from a marine compound, binds the minor groove of DNA and disrupts the cell cycle, which inhibits cell proliferation.45Trabectedin is approved in Europe and was also approved in the United States in October 201546for the treatment of liposarcoma and leiomyosarcoma in patients who previously received anthracycline-based chemotherapy, although it can also be used in other subtypes.8
Trabectedin received US FDA approval on the basis of a phase III clinical trial involving 518 patients with metastatic or recurrent leiomyosarcoma or liposarcoma.47Participants were randomly assigned to receive either trabectedin or dacarbazine. The patients receiving trabectedin experienced a PFS of about 4.2 months compared with only 1.5 months in patients assigned to dacarbazine (HR 0.55;P<.001). An interim analysis of OS showed a 13% reduction in risk of death in the trabectedin arm compared with dacarbazine (P= .37).47The most common grade 3 to 4 AEs were myelosuppression and transient elevation of transaminases in the trabectedin arm.
In an expanded access program, Samuels et al evaluated 807 patients with advanced STS who received trabectedin. Half of the patients had disease progression and the remaining half had a complete response (CR), partial response (PR), or stable disease (SD). ORRs were higher in patients with leiomyosarcomas or liposarcomas than in patients with other STS (5.7% vs 7.5% vs 4.0%, respectively). Leiomyosarcomas and liposarcomas (L-sarcomas) were also associated with better OS (16.2 vs 8.4 months, L-sarcomas vs other STS, respectively). The most common AEs were nausea, vomiting, constipation, increased liver enzymes, anemia, and neutropenia.45In separate retrospective studies, researchers found that fatigue and myelosuppression were reasons for discontinuation of trabectedin after 1 year of therapy.48In a study by Blay et al, trabectedin and doxorubicin-based chemotherapy did not demonstrate efficacy in translocation-related sarcomas.49
Trabectedin is recommended at a dose of 1.5 mg/m2given as an intravenous infusion over the course of 24 hours every 21 days until disease progression or unacceptable toxicity.50It is recommended that patients taking trabectedin have a normal bilirubin and aspartate aminotransferase and alanine aminotransferase levels of ≤2.5 times the upper limit of normal.
Eribulin, like trabectedin, is derived from a marine compound.51Eribulin stops cell proliferation by inhibiting the movement of microtubules, and has also demonstrated improved efficacy in liposarcoma and leiomyosarcoma when compared with other forms of STS. In a phase II study, Schöffski et al evaluated 128 patients with either adipocytic sarcoma, leiomyosarcoma, synovial sarcoma, or other sarcomas treated with eribulin 1.4 mg/m2 on days 1 and 8 every 3 weeks. The adipocytic sarcoma and leiomyosarcoma groups met the primary endpoint, and the 12-week PFS was 46.9% and 31.6%, respectively. Common grade 3 to 4 treatment-emergent AEs included neutropenia and leucopenia.
Eribulin was approved in January 2016 for patients with unresectable or metastatic liposarcoma who have received a prior anthracycline-based chemotherapy regimen.52The results were based on a phase III study by Schöffski et al in which eribulin was compared with dacarbazine.53Among 143 patients with liposarcoma, the OS was 15.6 months with eribulin compared with 8.4 months with dacarbazine.
In 452 patients with liposarcoma and leiomyosarcoma, patients receiving eribu­lin had an OS of 13.5 months compared with dacarbazine (11.5 months), but the difference was not significant (HR, 0.77;P= .017).54PFS was also not significantly different between the 2 groups. Grade ≥3 AEs were more common in the eribulin group than the dacarbazine group.
Targeted Therapy
Olaratumab, a platelet-derived PDGFR-alpha antagonist, was granted accelerated approval by the US FDA for the treatment of unresectable, advanced STS when given in combination with doxorubicin in October 2016.55Approval was also recommended by the European Medicines Agency's Committee for Medicinal Products for Human Use in September 2016.56The phase II trial that led to its approval showed a 48% reduction in the risk of death over doxorubicin monotherapy (HR, 0.52;P<.05).57OS was improved with the combination compared with doxorubicin (26.5 vs 14.7 months, respectively). PFS and ORR were also increased with the combination.
AEs were more frequent in the trial with the combination versus with doxorubicin alone. The AEs more frequently seen with the combination included neutropenia, mucositis, nausea, vomiting, and diarrhea. Grade 3 or higher febrile neutropenia was noticed in 13% of patients in the combination arm and in 14% of patients in the doxorubicin monotherapy arm.
Olaratumab is administered at 15 mg/kg intravenously over 60 minutes on days 1 and 8 of a 21-day cycle, with doxorubicin also given for the first 8 cycles.58It is recommended for patients with a histologic subtype for which an anthracycline-containing regimen is appropriate, and for patients whose tumors are not amenable to surgery or radiotherapy. Treatment with olaratumab and an anthracycline are also recommended in the frontline setting for metastatic or recurrent disease in a number of subtypes.59The agent had been granted fast track and breakthrough therapy designations and a priority review status from the FDA prior to its accelerated approval.60The phase III ANNOUNCE confirmation trial to verify the benefits of olaratumumab plus doxorubicin is ongoing and has already been fully accrued.61
Pazopanib, a second-line therapy, is an oral multitargeted tyrosine kinase receptor inhibitor and is approved to treat patients with non-adipocytic and non-GIST STS.62Specifically, pazopanib targets VEGF 1-3, fibroblast growth factor receptor 1 and 3, PDGF a and b, and KIT selectivity. In the phase III PALETTE trial, van der Graaf et al randomized 369 patients with advanced STS to receive pazopanib or placebo.63Pazopanib significantly improved PFS compared with placebo (4.6 vs 1.6 months, respectively; P <.0001). No differences in OS were found, and the majority of patients had SD. Only 6% of patients had a PR. In the same group of patients, Coens et al found that pazopanib did not improve or worsen health-related quality of life.64The most common AEs with pazopanib were fatigue, diarrhea, nausea, weight loss, and hypertension.
Using data from the PALETTE trial and a phase II trial, Kasper et al determined that 22% of patients were long-term responders and survivors with pazopanib.65This was defined as PFS,3of 6 months and OS,3of 18 months. A total of 12 patients (3.5%) were treated with pazopanib for >2 years, and favorable prognostic factors included good performance status, low or intermediate tumor grading, and normal hemoglobin level at baseline.