Erba Discusses the Diagnostic Workup and Laboratory Findings Signaling a Case of PV
Harry P. Erba, MD, PhD, recently shared the treatment considerations and decisions he makes when treating patients with polycythemia vera.
Harry P. Erba, MD, PhD

Harry P. Erba, MD, PhD
Harry P. Erba, MD, PhD, recently shared the treatment considerations and decisions he makes when treating patients with polycythemia vera (PV). Erba, professor of medicine, University of Alabama at Birmingham, explained his treatment decisions based on 2 case scenarios during aTargeted Oncologylive case-based peer perspectives dinner.
CASE 1February 2017
A 58-year-old man presented with symptoms of frequent headache and dizziness. He was being treated for hypertension at the time. Physical examination was unremarkable.
Lab findings showed:
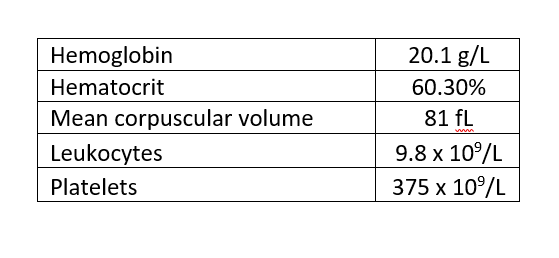
TARGETED ONCOLOGY:What are your initial impressions of this patient?
Erba:This is isolated hemoglobin hematocrit, and you need to evaluate the patient for volume depletion. So, is this a patient who has dehydration? It is unlikely, given the time course here. The patient has been having symptoms of headaches and dizziness, but dehydration can cause this. You have to look at whether the patient has hypoxia driving the elevated hemoglobin. There is chronic obstructive pulmonary disease or sleep apnea, or very rare things like high-affinity hemoglobin, pathologic causes of erythropoietin production like tumors or erythropoietin doping, and finally, erythropoietin-independent production of red cells. That is basically what PV is.
This case allows you to discuss the entire differential diagnosis from a pathophysiologic point of view. The other counts are not elevated, the patient does not have a big spleen, and they do not have any symptoms other than those related to having a high hemoglobin.
TARGETED ONCOLOGY:When should PV be suspected?
Erba:In a patient who has isolated elevated hemoglobin hematocrit, but also in patients with splenomegaly, patients with thrombotic eventsespecially rare ones, like Budd-Chiari syndrome—and then certain constitutional symptoms like aquagenic pruritus or bone pain where you're considering myeloprolific neoplasms.
TARGETED ONCOLOGY:What is the diagnostic workup?
Erba:You make sure the patient is not hypoxic. We usually talk about red blood cell mass studies and how those are hard to get anymore and not necessary to get for diagnostic criteria. It comes down to making sure the patient is not hypoxic by getting a blood gas or an oxygen saturation, getting a serum erythropoietin level, which should be suppressed in PV and normal and elevated in almost every other condition. Bone marrow biopsy is considered part of the World Health Organization criteria showing a panmyelosis. But if a patient has persistent elevation of the hematocrit, a positiveJAK2mutation, and a low erythropoietin level, you don't absolutely have to get that.
TARGETED ONCOLOGY:How do you evaluate prognostic risk in your PV patients at diagnosis?
Erba:If the patient has a history of thrombosis, is over age 60, or has other risk factors for cardiovascular disease. Leukocytosis is also considered a risk factor for thrombosis by some.
TARGETED ONCOLOGY:Discuss the treatment approach for a patient who is newly diagnosed with PV.
Erba:This is a patient who does not have constitutional symptoms, does not have splenomegaly, and does not have elevation of white cells or platelets, so the only manifestation of the disease is the PV and it's causing symptoms.
For a patient like this, phlebotomy to maintain hematocrit levels less than 35% and aspirin are the mainstay of therapy. You can think about adding cytoreductive therapy if a patient requires too many phlebotomies, is non-compliant with phlebotomies, develops symptomatic iron deficiency from the phlebotomies, develops symptomatic splenomegaly, or develops leukocytosis and thrombocytosis, but not all physicians use that as a reason for giving cytoreductive therapy. Finally, if the patient develops a thrombotic event, or as patients age, that would be a reason for starting cytoreductive therapy, typically with hydroxyurea [Hydrea] and, less commonly in the United States, with interferon.
CASE 2August 2014
A 62-year-old female presented with symptoms of aquagenic pruritus, night sweats, and left upper quadrant fullness. She was diagnosed withJAK2V617F-positive PV.
Her past medical history included unstable angina treated with angioplasty and a coronary artery stent 2 years ago. She has ongoing treatment for type 2 diabetes. Physical examination was remarkable for palpable splenomegaly.
TARGETED ONCOLOGY:Describe your initial impressions of this patient based on her presentation.
Erba:This is a patient who has PV with constitutional symptoms, night sweats, and aquagenic pruritus, so she is symptomatic from the disease. She has fullness in the left upper quadrant that she complains aboutthis is a symptom of splenomegaly. She has symptoms of PV, other than just the elevated hematocrit, and has symptoms from the splenomegaly, and on a physical exam you would see that.
In terms of past medical history, she has documented histories of cardiovascular disease requiring stent placement. That has cardiovascular risk factors, type 2 diabetes.
The initial impression is that this is a patient over the age of 60 who has risk factors for cardiovascular and thromboembolic events, so this is a patient I would consider for cytoreductive therapy with hydroxyurea, aspirin, and a phlebotomy to maintain the hematocrit below 45%.
February 2016
For 1.5 years, the patient was maintained on treatment with aspirin and hydroxyurea for 500 mg/day. She required 4 phlebotomies in the last 6 months. She still has palpable splenomegaly. Hydroxyurea was increased from 500 mg to 1,000 mg daily.
August 2016
No phlebotomies in the last 3 months. A physical exam was still remarkable for splenomegaly, but spleen tip now just at costal margin and non-tender. She has had a 3.5 cm, poorly healing distal leg ulcer for the last 2 months.
Lab findings showed:
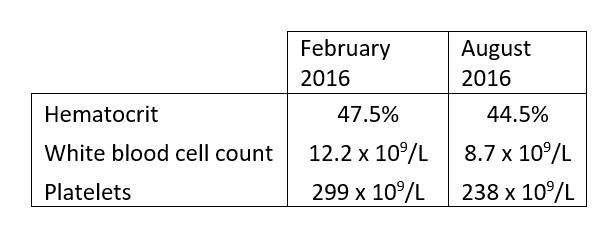
TARGETED ONCOLOGY:What are the criteria for intolerance to hydroxyurea?
Erba:The guidelines for what is considered resistance to hydroxyurea requires that a patient get the maximum tolerated dose or at least 2 grams of hydroxyurea per day for at least 3 months. This patient is not at the maximum tolerated dose, so you can go up on the dose of hydroxyurea, and it works. The phlebotomies have gone away and there is splenomegaly, but it's not tender and it's just at the costal margin. She had a nice response to titration by hydroxyurea. However, she has now developed a known complication of the hydroxyurea, which is a distal leg ulcer. Her counts are well controlled on the higher dose of hydroxyurea, 1000 mg/day.
There are a number of reasons for intolerance to hydroxyurea. There are hematologic reasons, meaning that you can't control the hematocrit or splenomegaly without dropping the absolute neutrophil count below 1000 or platelets below 100,000. There's also non-hematologic intolerance. Gastrointestinal toxicity is probably the most common, with nausea or vomiting, but also rare things like distal leg ulcers, fever, and pneumonitis are seen, as are an acceleration of the number and severity of squamous cell carcinomas of the skin. Those would be examples of intolerance.
Some investigators might consider decreasing the dose of hydroxyurea, but in my experience and that of many of my colleagues, we feel that you have to stop the hydroxyurea to get this to heal. Even if you were to go down on the dose, remember that the patient was not responding to the lower dose, so it doesn't make sense to go down. For this patient, we would consider her for ruxolitinib [Jafaki] therapy, based on that.
TARGETED ONCOLOGY:Which patients are not candidates for ruxolitinib?
Erba:









