Entrectinib Shows Durable Responses in ROS1-Positive NSCLC
The tyrosine kinase inhibitor entrectinib shows promising responses in patients with non–small cell lung cancer harboring a ROS1 mutation.
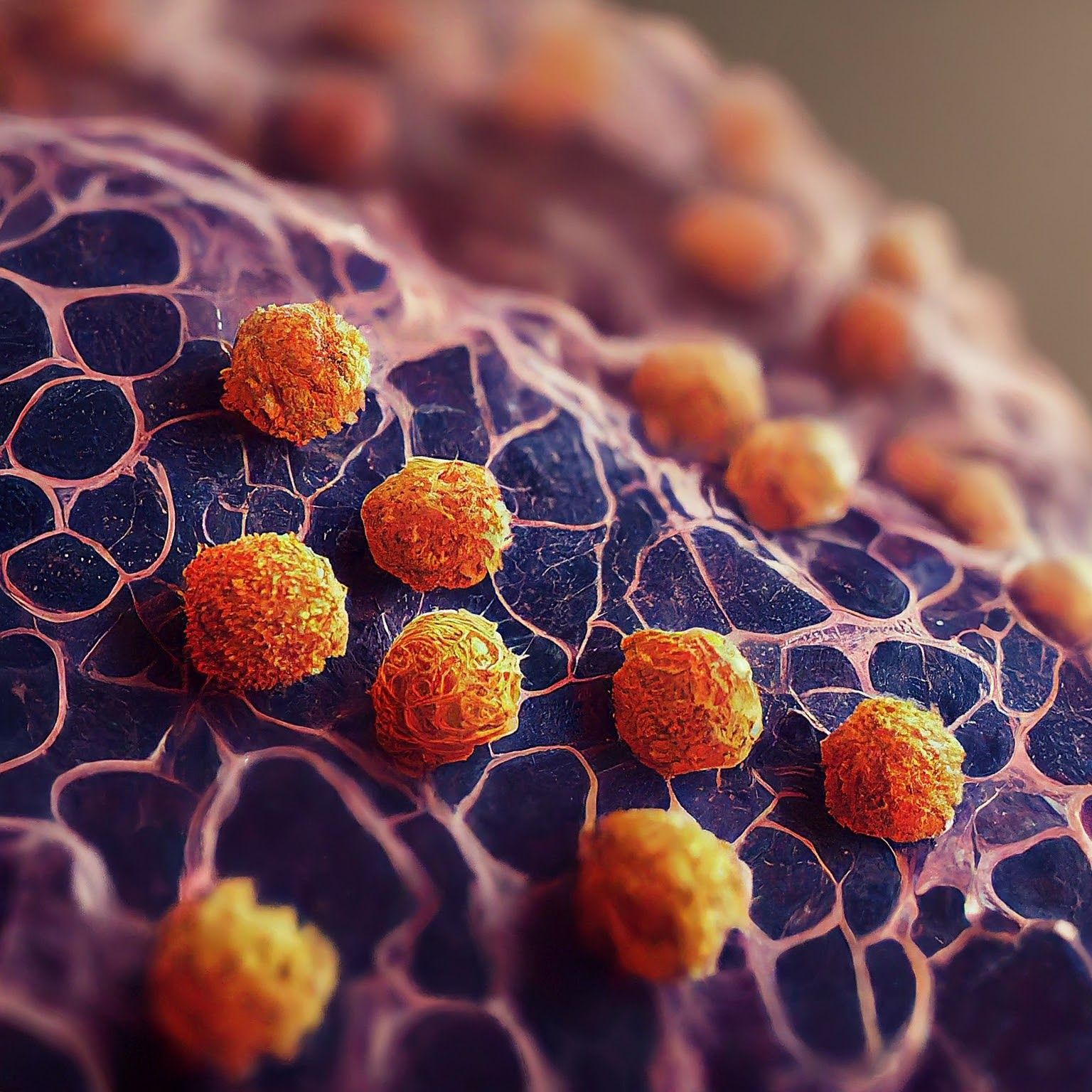
Microscopic image of non-small cell lung cancer - Generated with Google Gemini AI
Entrectinib (Rozlytrek) delivered durable responses and progression-free survival (PFS) rates in patients with ROS1-positive advanced/metastatic non–small cell lung cancer (NSCLC), according to findings from the phase 2/3 Blood First Assay Screening Trial (BFAST) study (NCT03178552) using liquid biopsy to identify targetable mutations.1,2
The objective response rate was 81.5% (95% CI, 68.6%-90.8%), and with a protocol-defined threshold was 70.4% (95% CI, 56.0%-82.0%), cohort D of the study (n = 55) met its primary end point. Two patients achieved a complete response and 42 achieved a partial response (PR) by investigator assessment. The clinical benefit rate by investigator was 87.0% (95% CI, 75.1%-94.6%). This was consistent with previously reported analyses of patients receiving entrectinib. Additionally, the median duration of response was 13.0 months (95% CI, 6.3-18.4) by investigator assessment.
Regarding PFS, the median was 12.9 months (95% CI, 8.7-18.5) by investigator assessment. At the cutoff, overall survival (OS) data were immature. The 12-month OS probability was 79.0%.

Importantly, the study found that the prevalence of ROS1 mutations by liquid biopsy was consistent with previous reports using tissue-based testing, “providing further evidence that liquid biopsies are an appropriate methodology for identification of patients who may benefit from entrectinib treatment,” according to study authors.1
Among the 4 (7.3%) patients with central nervous system (CNS) metastases, the median time to CNS progression was not reached, and the 12-month CNS PFS rate was 83.5% by investigator assessment. Of these 4 patients, 2 achieved PRs.
“Brain metastases occur in approximately 40% of patients with ROS1-positive, advanced NSCLC, and there is a need for CNS-active treatments for these patients. Entrectinib was specifically designed to penetrate the blood–brain barrier and has demonstrated activity within the CNS,” study authors explained.
The study included patients 18 years and older with unresectable stage IIIB or IV NSCLC and an ECOG performance status of 0 to 2. Multiple cohorts involving patients with other gene alterations were analyzed in BFAST. In this ROS1-positive cohort, 55 of the 92 included patients were treatment naive. At the time of the primary analysis, 32 patients (58%) remained in the study and 15 (27%) were still undergoing therapy.
Most treatment-related adverse events (TRAEs) reported were not serious, and no deaths were attributed to treatment. A total of 7 patients (12.7%) experienced 1 or more serious TRAEs, including cerebellar syndrome, cognitive disorder, memory impairment, cardiac failure, left ventricular dysfunction, interstitial lung disease, pleural effusion, ankle fracture, and fluid retention.Weight gain was the most common grade 3 to 5 AE, with 7.3% of patients (n = 4) experiencing this; all incidences were grade 3. AEs led to treatment discontinuation in 4 (7.3%) patients. This safety profile is consistent with what has been previously reported about entrectinib.