Eftilagimod Alpha is Safe, Shows Improved Overall Survival in mBC
The phase 2b AIPAC study, Eftilagimod alpha was found to improve overall survival in metastatic breast cancer along with a tolerable safety profile.
Eftilagimod alpha (IMP321 efti), a soluble LAG-3 protein, in combination with weekly paclitaxel was found to significantly improve overall survival (OS) in patients with metastatic breast cancer, according to final OS results of the phase 2b AIPAC study presented at the Society for Immunotherapy of Cancer Annual Meeting 2021.
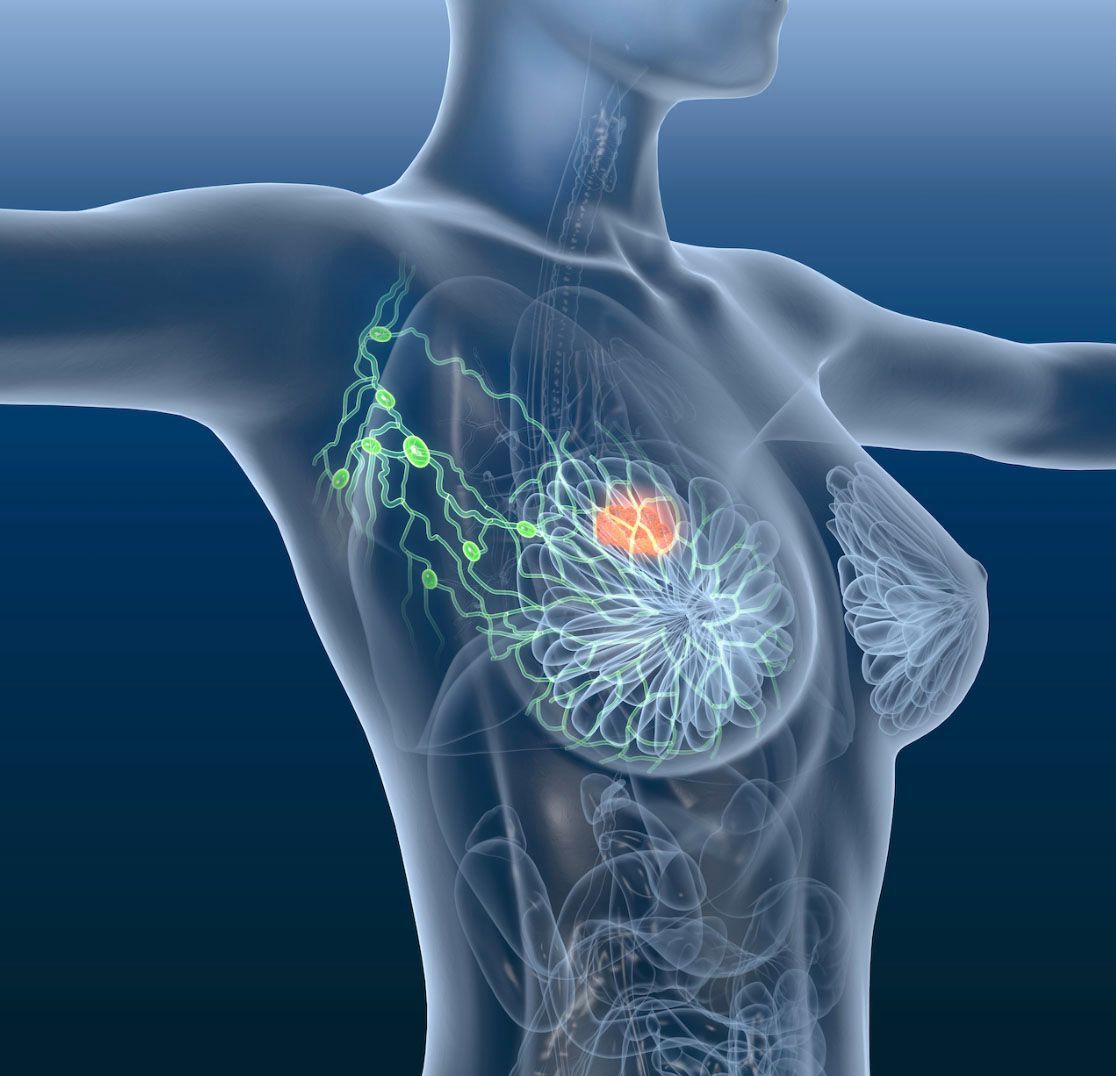
Efti is designed to target a subset of MHC class 2 molecules, mediating antigen presenting cell and CD8 T-cell activation. This is meant to stimulate the dendritic cell network and cause T-cell recruitment, leading to stronger anti-tumor responses in combination with paclitaxel then is what is commonly observed with paclitaxel alone.
The phase 2b AIPAC study (NCT02614833) evaluated efti in combination with paclitaxel in patients with metastatic breast carcinoma. The primary end points of the study are the recommended phase 2 dose and progression-free survival. Secondary end points include safety and tolerability, overall survival, pharmacokinetics, change in quality of life, evaluation of time to next treatment, and objective response rate, and the evaluation of stable disease.
During the study patients with HR-positive metastatic breast cancer were randomized 1:1 to either receive the experimental combination of chemotherapy and efti or the control combination of chemotherapy and a placebo for 24 weeks. After the treatment phase, patients will receive either the immunotherapy agent or the placebo for 48 weeks.
In the overall population (n = 226), the median age was 60 (range, 24-87) and the median BMI was 24.7 (range, 15.4-48.1). Additionally, 61.5% had an ECOG score of 0 and 91.6% had visceral disease. Prior therapies included surgery (82.3%), radiotherapy (77%), systemic therapy (94.7%), adjuvant therapy (73.5%), and therapy for metastatic disease (69.9%). Forty-two percent of patients received a prior taxane, 44.2% received a prior CDK4/6, and 91.6% received a prior endocrine therapy. Nearly 85% of patients were endocrine resistant. Prior to inclusion in the study, 74.8% received a palliative therapy.
The median age of the experimental group (n = 114) was 56 (range, 24-87) and the median BMI was 24.7 (range, 18.1-48.1) and 60.5% had an ECOG score of 0. Visceral disease was seen in 90.5% of patients. Prior therapies included surgery (80.7%), radiotherapy (76.3%), systemic therapy (93%), adjuvant therapy (74.6%), and therapy for metastatic disease (68%). Forty-five percent of patients received a prior taxane, 44.6% received a prior CDK4/6, and 90.4% received a prior endocrine therapy, with 82.5% of patients being endocrine resistant. At the time of inclusion, 72.8% of patients’ last therapy was palliative.
In the control group (n = 112), the median age was 61 years (range, 35-79) and the median BMI was 24.9 (range, 15.4-44.5). Sixty-three percent of patients had an ECOG score of 0, and visceral disease was seen in 92.9% of patients. Prior therapies included surgery (83.9%), radiotherapy (77.7%), systemic therapy (96.4%), adjuvant therapy (72.3%), and prior therapy for metastatic disease (71.4%). Additionally, 38.4% of patients received a prior taxane, 43.9% received a prior CDK4/6, and 92.9% received a prior endocrine therapy, of which 85.6% of patients were resistant too. At the time of inclusion, the last prior line of therapy was palliative for 76.8% of patients.
At the minimum follow-up of 22 months, there was an OS increase of a median of 2.9 months. The median OS of patients in the placebo group was 17.5 months (95% CI, 12.9-21.9) compared with 20.4 months in the efti group (95% CI, 14.3-25.1. Additionally, a significant deterioration of quality of life was seen in the placebo group at 6 months, where quality of life was stable in the experimental group. Additionally, an increase in pre-dose CD8 T cells was found to significantly correlate to overall survival.
Ninety-nine percent of patients in the experimental group and 100% of patients in the control arm experienced at least one treatment-emergent adverse event (TEAE). TEAE’s led to death in 1.8% of patients in the experimental group and 2.7% of patients in the control arm. Additionally, TEAEs led to discontinuation in 5.3% of patients in the experimental arm and 6.3% of patients in the control arm. One or more grade 3 or higher TEAE’s were seen in 68.4% of patients in the experimental arm versus 65.2% of patients in the control arm. The most common efti-related AEs were injection related reaction, which occurred in 65.8% of patients in the experimental arm versus 11.6% of patients in the placebo arm.
“Efti added to paclitaxel led to a non-significant 2.9 months median OS increase in predominantly endocrine resistant HR-positive HER2neu/- MBC patients. Results were significant in predefined subgroups which are in line with the mechanism of action of efti. This is one of the first trials to report efficacy of chemotherapy after introduction of CDK 4/6 inhibitors in previous treatment lines,” said AIPAC principle investigator Hans Wildiers, MD, of University Hospitals. “It underlines the high unmet medical need in this patient population. Based on the excellent safety profile of efti and the high unmet medical need a phase III study of efti plus weekly paclitaxel is warranted.”