Current Applications of Artificial Intelligence in Oncology
As we better understand the use of artificial intelligence in oncology, experts can improve outcomes, develop approaches to solve problems, advance the development of treatments that are made available to patients with cancer, and more.
Image Credit: © ipopba [stock.adobe.com]

The evolution of artificial intelligence (AI) is reshaping the field of oncology by providing new devices to detect cancer, individualize treatments, manage patients, and more.
Given the large number of patients diagnosed with cancer and amount of data produced during cancer treatment, interest in the application of AI to improve oncologic care is expanding and holds potential.
Tufia C. Haddad, M.D.

“An aspect of care delivery where AI is exciting and holds so much promise is democratizing knowledge and access to knowledge. Generating more data, bringing together the patient data with our knowledge and research, and developing these advanced clinical decision support systems that use AI are going to be ways in which we can make sure clinicians can provide the best care for each individual patient,” Tufia C. Haddad, MD, told Targeted OncologyTM.
While cancer treatment options have only improved over past decades, there is an unmet medical need to make these cancer treatments more affordable and personalized for each patient with cancer.1
As we continue to learn about and better understand the use of AI in oncology, experts can improve outcomes, develop approaches to solve problems in the space, and advance the development of treatments that are made available to patients.
Defining AI
AI is a branch of computer science which works with the simulation of intelligent behavior in computers. These computers follow algorithms which are established by humans or learned by the computer to support decisions and complete certain tasks. Under the AI umbrella lay important subfields.
Machine learning is the process in which a computer can improve its own performance by consistently utilizing newly-generated data into an already existing iterative model. According to the FDA, 1 of the potential benefits of machine learning is its ability to create new insights from the vast amount of data generated during the delivery of health care every day.2
“Sometimes, we can use machine learning techniques in a way where we are training the computer to, for example, discern benign pathology, benign pathology from malignant pathology, and so we train the computer with annotated datasets, where we are showing the different images of benign vs malignancy. Ultimately, the computer will bring forward an algorithm that we then take separate data sets that are no longer labeled as benign or malignant. Then we continue to train that algorithm and fine tune the algorithm,” said Haddad, medical oncologist, associate professor of oncology at the Rochester Minnesota Campus of the Mayo Clinic.
Deep learning is a smaller part of machine learning where mathematical algorithms are installed using multi-layered computational units which resemble human cognition. These include neural networks with different architeture types including recurrent neural networks, convolutional neural network, and long short-term memory.
Danielle S. Bitterman, MD

“Many of the applications integrated into commercial systems are proprietary, so it is hard to know what specific AI methods underlie their system. For some applications, even simple rules-based systems still hold value. However, the recent surge in AI advances is primarily driven by more advanced machine learning methods, especially neural network-based deep learning, in which the AI teaches itself to learn patterns from complex data,” Danielle S. Bitterman, MD, told Targeted OncologyTM. “For many applications, deep learning methods have better performance, but come at a trade-off of being “black boxes”, meaning it is difficult for humans to understand how they arrive at their decision. This creates new challenges for safety, trust, and reliability.”
Utilizing AI is important as the capacity the human brain must process information is limited, causing an urgent need for the implementation of alternative strategies to process big data. With machine learning and AI, clinicians can obtain increased availability of data, and boost the augmentation of storage and computing power.
Current Uses of AI in Oncology
As of October 5, 2022, the FDA had approved 521 medical devices which utilize AI and/or machine learning, with the majority of devices in the radiology space.2
“Primarily, where it is being more robustly developed and, in some cases, now, at the point of receiving FDA approval and starting to be applied and utilized in the hospitals and clinics, is in the cancer diagnostic space. This includes algorithms to help improve the efficiency and accuracy of, for example, interpreting mammograms. Radiology services, and to some extent, pathology, are where some of these machine learning and deep learning algorithms and AI models are being used,” said Haddad.
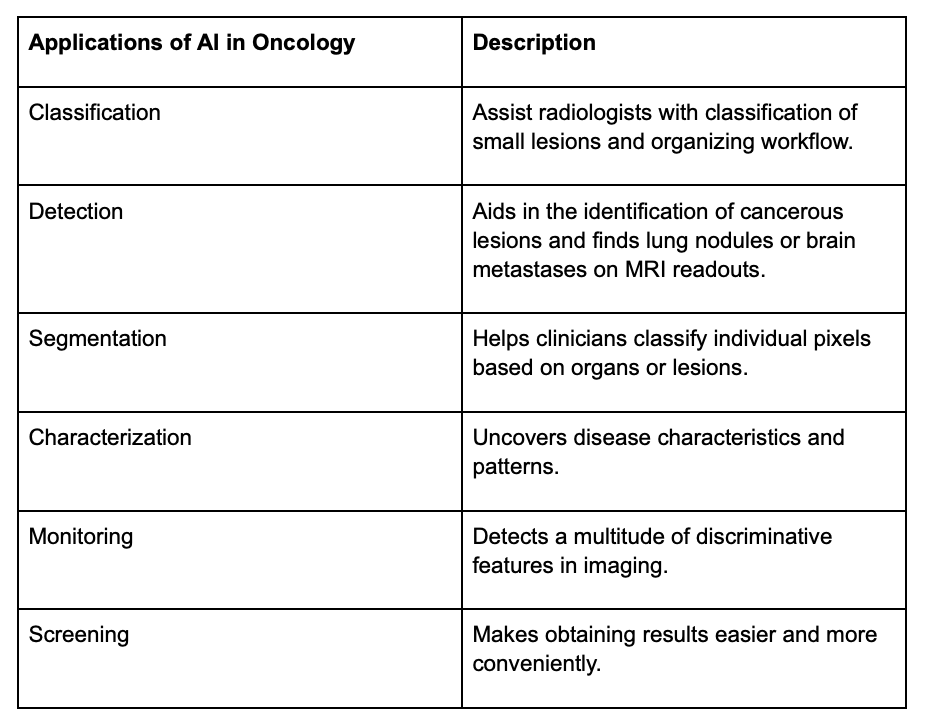
In radiology, there are many applications of AI, including deep learning algorithms to analyze imaging data that is obtained during routine cancer care. According to Haddad, some of this can include evaluating disease classification, detection, segmentation, characterization, and monitoring a patient with cancer.
Matthew A. Manning, MD
According to radiation oncologist Matthew A. Manning, MD, AI is already a backbone of some clinical decision support tools.
“The use of AI in oncology is rapidly increasing, and it has the potential to revolutionize cancer diagnosis, treatment, and research. It helps with driving automation… In radiation oncology, there are different medical record platforms necessary for the practice that are often separate from the hospital medical record. Creating these interfaces that allow reductions in the redundancy of work for both clinicians and administrative staff is important. Tools using AI and business intelligence are accelerating our efforts in radiation oncology,” Manning, former chief of Oncology at Cone Health, told Targeted OncologyTM, in an interview.
Understaning AI Use
Through combining AI human power, mamography screening has been improved for patients with breast cancer. Additionally, deep learning models were trained to classify and detect disease subtypes based on images and genetic data.
To find lung nodules or brain metastases on MRI readouts, AI uses bounding boxes to locate a lesion or object of interest and classify them. Detection using AI supports physicians when they read medical images.
Segmentation involves recognizing these lesions and accessing its volume and size to classify individual pixels based on organ or lesions. Examples of this are brain gliomas as they require quantitative metrics for their management, risk stratification and prognostication.
Deep learning methods have been applied to medical images to determine a large number of features that are undetectable by humans.3 An example of using AI to characteroze tumor come from the study of radiomics, which studies combines disease features with clinicogenomic information. This methods can inform models that successfully predict treatment response and/or adverse effects from cancer treatments.
Radiomics can be applied to a variety of cancer types, including liver, brain, and lung tumors. According to research in Future Science OA1, deep learning using radiomic features from brain MRI also can help differentiate brain gliomas from brain metastasis with similar performance to trained neuroradiologists.
Utilizing AI can dramatically change the ways patients with cancer are monitored. It can detect a multitude of discriminative features in imaging that by humans, are unreadable. One process that is normally performed by radiologists and that plays a major role in determining patient outcomes is measuring how tumors react to cancer treatment.4 However, the process is known to be labor-intensive, subjective, and prone to inconsistency.
To try and alleviate this frequent problem, researchers developed a deep learning-based method that is able to automatically annotate tumors in patients with cancer. Using a small study, researchers from Johns Hopkins Kimmel Comprehensive Cancer Center and its Bloomberg~Kimmel Institute for Cancer Immunotherapy successfully trained a machine learning algorithm to predict which patients with melanoma would respond to treatment and which would not respond. This open-source program, DeepTCR, was valuable as a predictive tool and helped researchers understand the biological mechanisms and responses to immunotherapy.
This program can also help clinicians monitor patients by stratifying patient outcomes, identifying predictive features, and helping them manage patients with the best treatments.
Proper screening for early diagnosis and treatment is a big factor when combating cancer. In the current space, AI makes obtaining results easier and more convenient.
“One of the important things to think about AI or the capabilities of AI in oncology is the ability to see what the human eye and the human mind cannot see or interpret today. It is gathering all these different data points and developing or recognizing patterns in the data to help with interpretation. This can augment some of the accuracy for cancer diagnostics.” added Haddad.
AI may also provide faster, more accurate results, especially in breast cancer screening. While the incorporation of AI into screening methods is a relatively new and emerging field, it is promising in the early detection of breast cancer, thus resulting in a better prognosis of the condition. For patients with breast cancer, a mammography is the most popular method of breast cancer screening.
Another example of AI in the current treatment landscape for patients with colon cancer is the colonoscopy. Colon cancer screening utilizes a camera to give the gastroenterologist the ability to see inside the colon and bowel. By taking those images, and applying machine learning, deep learning neural network techniques, there is an ability to develop algorithms to not only help to better detect polyps or print precancerous lesions, but also to discern from early-stage or advanced cancers.
In addition, deep learning models can also help clinicians predict the future development of cancer and some AI applications are already being implemented in clinical practice. With further development, as well as refinement of the already created devices, AI will be further applied.
“In terms of improving cancer screening, AI has been applied in radiology to analyze and identify tumors on scans. In the current state, AI is making its way into computer-assisted detection on diagnostic films. Looking at a chest CT, trying to find a small nodule, we see that AI is very powerful at finding spots that maybe the human eye may miss. In terms of radiation oncology, we anticipate AI will be very useful ultimately in the setting of clinical decision support,” said Manning.
AI for Clinicians
For oncologists, the emergence of the COVID-19 pandemic and time spent working on clinical documentation has only heightened the feeling of burnout. However, Haddad notes that a potential solution to help mitigate feelings of burnout is the development and integration of precision technologies, including AI, as they can help reduce the large amount of workload and increase productivity.
“There are challenges with workforce shortages as a consequence of the COVID-19 pandemic with a lot of burnout at unprecedented rates. Thinking about how artificial intelligence can help make [clinicians] jobs easier and make them more efficient. There are smart hospitals, smart clinic rooms, where just from the ingestion of voice, conversations can be translated to the physician and patient into clinical documentation to help reduce the time that clinicians need to be spending doing the tedious work that we know contributes to burnout, including doing the clinical documentation, prior authorizations, order sets, etc,” said Haddad.
Numerous studies have been published regarding the potential of machine learning and AI for the prognostication of cancer. Results from these trials have suggested that the performance and productivity of oncologists can be improved with the use of AI.5
An example is with the prediction of recurrences and overall survival. Deep learning can enhance precision medicine and improve clinical decisions, and with this, oncologists may feel emotional satisfaction, reduced depersonalization, and increased professional efficacy. This leaves clinicians with the potential of increased job satisfaction and a reduced feeling of burnout.
Research also has highlighted that the intense workload contributes to occupational stress. This in turn has a negative effect on the quality of care that is offered to patients.
Additionally, it has been reported that administrative tasks, such as collecting clinical, billing, or insurance information, contribute to the workload faced by clinicians, and this leads to a significantly limited time for direct face-to-face interaction between patients and their physicians. Thus, AI has helped significantly reduce this administrative burden.
Overall, if clinicians can do less of the tedious clerical work and spend more time doing the things they were trained to do, like having time with the patient, their overall outlook on their job will be more positive.
“AI will help to see that joy restored and to have a better experience for our patient. I believe that AI is going to transform most aspects of medicine over the coming years. Cancer care is extremely complex and generates huge amounts of varied digital data which can be tapped into by computational methods. Lower-level tasks, such as scheduling and triaging patient messages will become increasingly automated. I think we will increasingly see clinical decision-support applications providing diagnostic and treatment recommendations to physicians. AI may also be able to generate novel insights that change our overall approach to managing cancers,” said Haddad.
Impending Role of AI
While there have been increasing amounts of updates and developments for AI in the oncology space, according to Bitterman, a large gap remains between AI research and what is already being used.
To bridge this gap, Bitterman notes that there must be further understanding by both clinicians and patients regarding how to properly interact with AI applications, and best optimize interactions for safety, reliability, and trust.
“Digital data is still very siloed within institutions, and so regulatory changes are going to be needed before we can realize the full value of AI. We also need better standards and methods to assess bias and generalizability of AI systems to make sure that advances in AI don’t leave minority populations behind and worsen health inequities.”
Additionally, there is a concern that patients’ voices are being left out of the AI conversation. According to Bitterman, AI applications are developed by using patients’ data, and as a result, this will likely transform their care journey. To further improve the use of AI for patients with cancer, it is key to get the opinions from patients.
With further research, it should be possible to overcome the current challenges being faced with AI to continue to improve its use, make AI more popular, and improve the overall quality-of-life for patients with cancer.
“We need to engage patients at every step of the AI development/implementation lifecycle, and make sure that we are developing applications that are patient-centered and prioritize trust, safety, and patients’ lived experiences,” concluded Bitterman.