CRX100 Delivers Responses and Tolerability in Platinum-Resistant Ovarian Cancer
Ex vivo generation of CD3-positive, CD56-positive Natural Killer-Like (NKT) with CRX100 was successful in all 7 patients with ovarian cancer in a phase 1 trial.
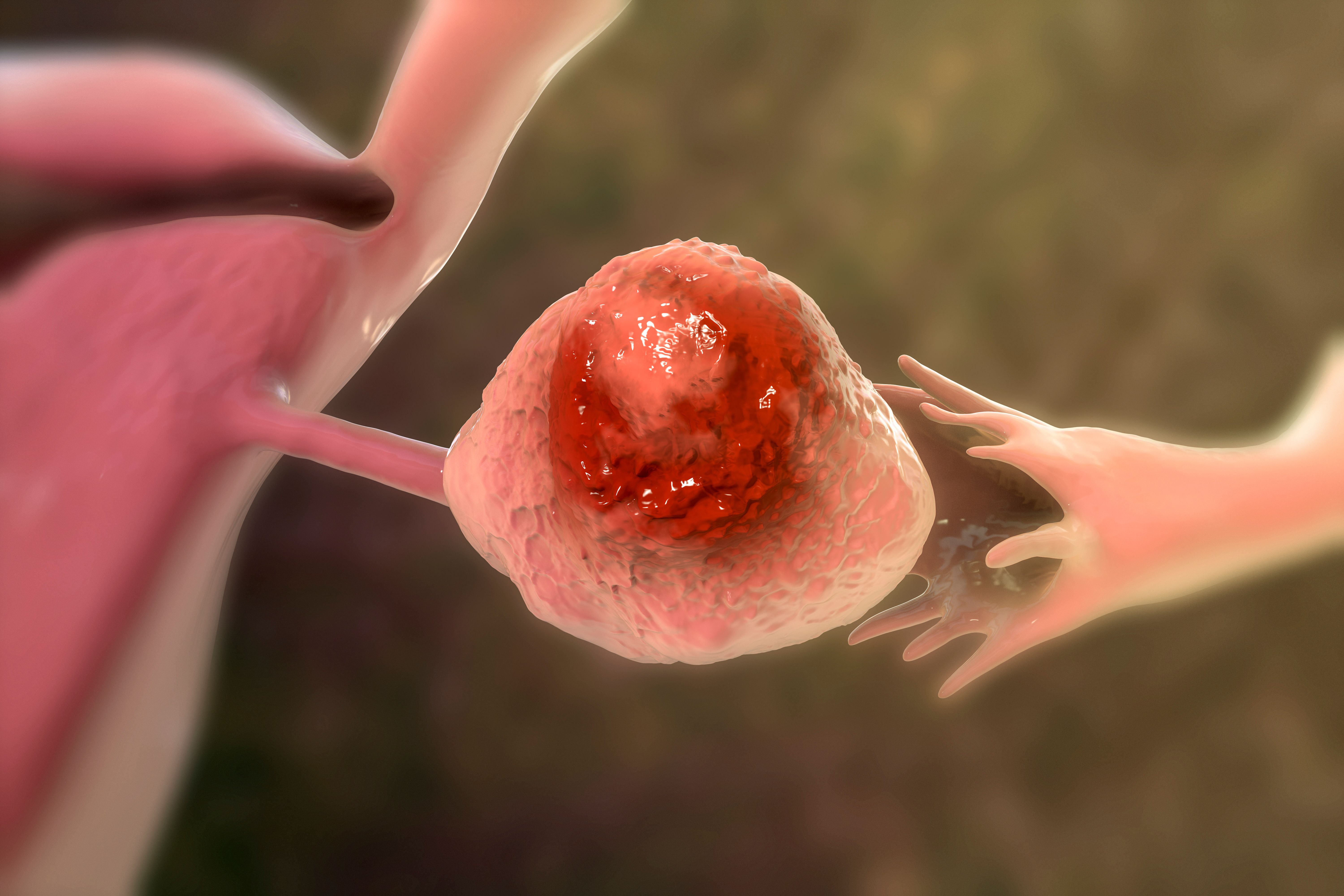
Illustration of ovarian caner: ©Dr_Microbe - stock.adobe.com
The combination of the novel adoptive natural killer-like T (NK-T) cell therapy CRX100 with oncolytic vaccinia virus demonstrated tolerability and conferred responses in a small cohort of patients with recurrent platinum-resistant ovarian cancer, according to findings from a phase 1 trial (NCT04282044) presented as a poster at the Society of Gynecologic Oncology (SGO) 2024 Annual Meeting on Women’s Cancer.1
Investigators reported stable disease in 1 patient who received an initial dose of 1E8 plaque-forming units (PFUs) of vaccinia plus 2-5E9 NK-T cells. Additionally, the patient had reduced tumor burden following a second dose of CRX100. This patient received subsequent treatment with an experimental antibody-drug conjugate plus pembrolizumab (Keytruda), which reduced CA125 serum marker levels to 296 U/mL.
Of 7 patients, 5 were alive at 1 to 36 months following treatment with CRX100. Two patients died due to progressive disease.
Findings highlighted that interferon-γ levels increased with study treatment, suggesting that CRX100 may produce an inflammatory tumor microenvironment that can delay antitumor responses and augment subsequent immunotherapy activity.
“This is the first in human trial using adoptive NK-T cell transfer combined with an oncolytic vaccinia virus,” Oliver Dorigo, MD, PhD, a Mary Lake Professor in Obstetrics & Gynecology – Gynecologic Oncology at Stanford Women’s Cancer Center, Stanford University and coauthors, wrote in the poster.
“The treatment with CRX100 was well tolerated and induced both clinical and immunological responses in patients with recurrent platinum resistant ovarian cancer. Based on our clinical observations and translational data, we are currently developing an expansion protocol that will include lymphodepletion prior to CRX100 treatment, and immune checkpoint inhibition to amplify antitumor cellular immune responses in the tumor microenvironment.”
Investigators of this ongoing phase 1 trial assessed 16 patients with various solid tumors, including 7 with ovarian cancer, 7 with colorectal cancer (CRC), and 2 with triple-negative breast cancer.
Patients underwent leukapheresis for generating autologous cytokine induced killer (CIK) killer cells, in which peripheral blood mononuclear cells expanded with interferon-γ and anti-CD38 antibodies before activation with interleukin-2 (IL-2). This process then yielded enrichment of CD3-positive, CD56-positive NK-T cells.
At approximately 21 days following apheresis, CIK cells at a target dose of 3E9 (range, 2-5E9) were administered in combination with vaccinia at 3E7, 1E8, 3E8, 1E9, or 3E9 PFUs per infusion before intravenous cell transfer. Four patients, including 2 with ovarian cancer and 2 others with CRC, required a second infusion due to safety, tolerability, and response outcomes observed during their first cycle.
The trial’s primary end points include treatment-emergent adverse effects (TEAEs) and dose-limiting toxicities as well as the maximum-tolerated dose and recommended phase 1b/2a dose.2 Secondary end points include immune responses based on levels of neutralizing antibodies and early antitumor activity per iRECIST criteria.
Patients 18 years and older with histologically confirmed triple-negative adenocarcinoma of the breast, adenocarcinoma of the colon or rectum, hepatocellular carcinoma, epithelial ovarian cancer, malignant melanoma, non-small cell lung cancer, or gastric cancer are eligible for enrollment. Those with ovarian cancer must have received at least 1 prior line of treatment with standard of care including a platinum-containing regimen for relapsed/refractory disease to enroll on the trial.
Concerning the current ovarian cancer cohort, 5 patients were White, and 5 were not Hispanic or Latino.1 Patients received anywhere from 5 to 13 prior lines of treatment, and all were previously treated with chemotherapy.
Investigators reported successful ex vivo generation of CD3-positive, CD56-positive NK-T cells in all patients with ovarian cancer. Additionally, there were no dose-limiting toxicities. The most common AE was grade 1 fever, and findings highlighted a single grade 3 AE, which was fatigue. Six AEs were determined to be serious AEs, although none of these toxicities led to dose modification of CRX100.