CNS-PFS Prolonged With Tucatinib Plus Palbociclib/Letrozole in HR+/HER2+ Breast Cancer
A non-chemotherapy–based targeted regimen comprised of tucatinib, palbociclib, and letrozole was found to prolong central nervous system (CNS) progression-free survival (PFS) in patients with hormone receptor–positive, HER2-positive breast cancer.
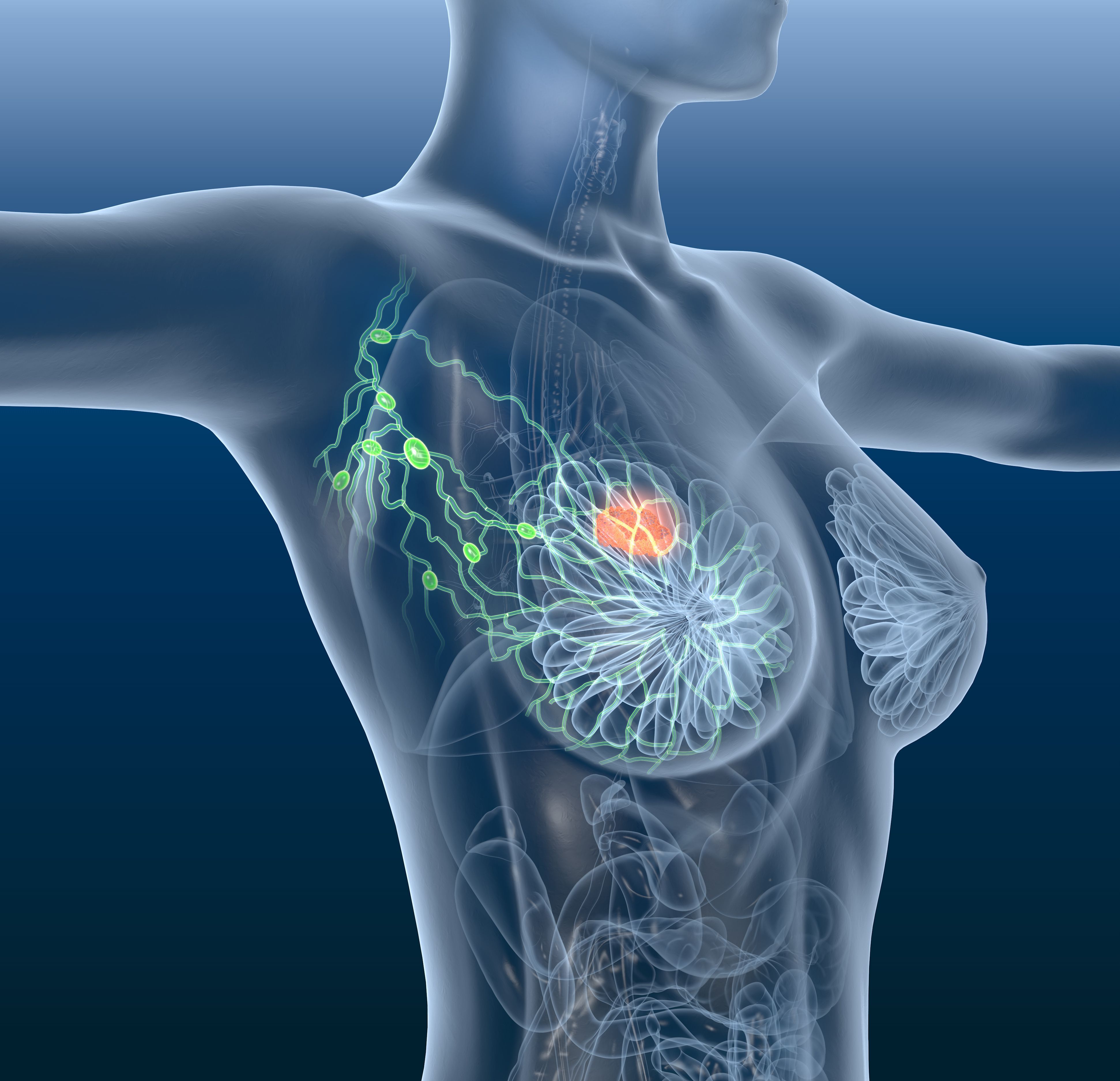
Prolonged central nervous system (CNS) progression-free survival (PFS) in patients with hormone receptor–positive, HER2-positive breast cancer was observed with a non-chemotherapy–based targeted regimen comprised of tucatinib (Tukysa), palbociclib (Ibrance), and letrozole, according to data from an exploratory analysis of a phase 1b/2 trial (NCT03054363).1
Results, which were presented during the 2021 San Antonio Breast Cancer Symposium, showed that in 15 patients with CNS metastases, the median CNS-PFS was 8 months with the triplet regimen. Additionally, the 1-year CNS-PFS rate in these patients was 20% (n = 3), and the 2-year CNS-PFS rate was 13% (n = 2).
“The majority of patients had treated (non-measurable) CNS lesions, limiting the evaluation of CNS response and biasing outcome towards stable disease [SD],” lead study author Elena Shagisultanova, MD, PhD, of the University of Colorado Cancer Center, and colleagues, wrote in a poster on the data. “Moreover, we demonstrate the ability to get prolonged clinical benefit with this regimen post first CNS progression in carefully adjudicated cases.”
For the trial, investigators examined the combination of a HER2-targeted TKI, a CDK4/6 inhibitor, and an anti-hormonal agent in patients with hormone receptor–positive, HER2-negative metastatic breast cancer who had untreated asymptomatic or treated stable CNS metastases.
To be eligible for enrollment, patients needed to be post-menopausal or premenopausal on ovarian suppression. Moreover, they must have received 2 or more HER2 inhibitors at any time of their disease, 1 or more HER2-targeted agents in the metastatic setting, and up to 2 endocrine agents for metastatic disease. Patients were allowed to have received prior treatment with letrozole. However, if patients received prior treatment with HER2 TKIs or CDK4/6 inhibitors, they were excluded.
Study participants received tucatinib at a twice-daily dose of 300 mg, palbociclib at a daily dose of 125 mg for 21 days on and 7 days off, and letrozole at a daily dose of 2.5 mg. Efficacy was evaluated using RANO-BM and RECIST v1.1 criteria and based on investigator assessment. Moreover, investigators examined CNS-PFS, which was defined as intracranial progression or death, and bi-compartmental PFS.
Previous results from the trial showed that the combination had an acceptable safety profile and encouraging antitumor activity in this population.2 In the poster shared during the 2021 SABC, investigators reported data from an exploratory analysis of intracranial efficacy in patients who had CNS metastases.
Within the 15 patients with CNS MTS, the mean age was 47 years (range, 22-70), and the mean number of prior lines of therapy received for metastatic disease was 2 (range, 1-5). Additionally, 9 patients (60%) received prior CNS radiation, 1 patient (7%) underwent neurosurgery alone, 3 patients (20%) underwent neurosurgery and radiation, and 2 patients (13%) did not receive any prior treatment for CNS disease. All patients had previously received HER2-targeted therapy with trastuzumab (Herceptin) and pertuzumab (Perjeta), and 5 patients received ado-trastuzumab emtansine (T-DM1; Kadcyla).
Of the 15 patients enrolled to the trial, 14 were evaluable for disease; 1 patient was determined to have non-evaluable disease because they had no evidence of disease in the CNS for 24 months. At a data cutoff date of November 1, 2021, 12 patients had received treatment; 5 of these patients had SD for 6 months or longer with the combination, 6 had SD for less than 6 months, and 1 experienced a complete response.
Two patients were not treated; 1 patient who had a non-measurable dural lesion had SD for 5 months, and the other patient had a measurable lesion and had SD for 8 months.
Regarding safety, prior data showed that the most common grade 3 or higher adverse effects (AEs) reported with the triplet regimen included neutropenia (58%), leukopenia (24%), diarrhea (17%), and fatigue (14%). Notably, these AEs were determined to be manageable. Moreover, no cases of cerebral edema were reported in patients with CNS metastases, including those who received radiation for isolated CNS progression during the study.










