Challenges Abound With Immunotherapy Biomarkers
Checkpoint inhibition has demonstrated efficacy for the treatment of melanoma in several clinical trials. However, biomarkers to predict safety and efficacy of immunotherapies in individual melanoma patients are lacking.
Checkpoint inhibition has demonstrated efficacy for the treatment of melanoma in several clinical trials. However, biomarkers to predict safety and efficacy of immunotherapies in individual melanoma patients are lacking.
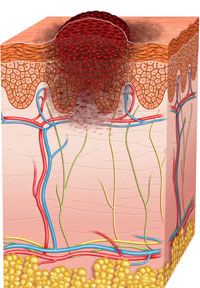
Checkpoint inhibition has demonstrated efficacy for the treatment of melanoma in several clinical trials.1-4However, biomarkers to predict safety and efficacy of immunotherapies in individual melanoma patients are lacking.
There is an urgent need for prognostic biomarkers to predict patient responses to specific therapies for melanoma in order to provide safe and effective treatment options. Concurrent treatment of patients with the programmed cell death-1 (PD-1) inhibitor nivolumab and ipilimumab, an antibody against cytotoxic T-lymphocyte-associated protein 4 (CTLA-4), has resulted in significant side effects while combination treatment with ipilimumab and the oncolytic virus talimogene laherparepvec (T-VEC) has shown better tolerability.5
The identification of biomarkers for response to checkpoint inhibition in melanoma is in the early stages of development. Several checkpoint inhibitors have been targeted by companies using antibodies. In addition to nivolumab and ipilimumab, the anti-PD-1 antibody pembrolizumab and antibodies targeting programmed death ligand 1 (PD-L1), MEDI4736 and MPDL3280A, have generated excitement for their antitumor responses in melanoma.6However, the use of these checkpoint inhibitors as prognostic biomarkers for treatment response remains in question.7
There are several challenges to consider when systematically evaluating potential biomarkers. Some of these include protocols for processing tissue samples, standardization of biomarker testing, and timing cutoffs for data interpretation.8
Choosing the proper tissue samples and processing protocol is critical for identifying biomarkers for any disease. First, the source of the tumor sample, primary or metastatic disease, must be determined.9Tumor heterogeneity and the possibility of the presence of multiple tumors are added levels of complexity when acquiring tissue samples.9 Another consideration includes the method of biopsy for tissue collecting: excisional, core, or fine needle aspiration.9Finally, the tissue sample must either be frozen or formalin-fixed, paraffin embedded for biomarker measurement. Different assays may require different tissue processing.10
In order to conduct a high-powered study to determine the clinical implications of candidate biomarkers for melanoma, common assays must be adopted, including standardized antibody and tissue staining conditions for immunohistochemistry.10Measuring assay output manually or in an automated fashion must also be determined.9
Part of the reason that the use of PD-L1 as a prognostic biomarker remains unknown is the lack of standardization of PD-L1 testing by various organizations. Mario Sznol, MD, of Yale Cancer Center in New Haven, Connecticut stated, “Multiple assays are in development for PD-L1 by drug companies. It is confusing to know which assay to use.”11
Defining standardized cutoffs between biopsy and treatment for evaluating positive results is critical for determining the prognostic value of a biomarker.8,12Biomarker expression may be time or therapy dependent, and measurements need to be taken at optimal times in order to determine the relevance of a potential biomarker’s expression to treatment response.12
Additionally, the effects of other previous or concomitant treatments must be taken into account when evaluating the utility of a potential biomarker.9Researchers must take care to consider patient histories when selecting samples for biomarker testing, because particular treatments or variation among patient histories may confound testing results.
Finally, details of immunohistochemical staining may be indicative of patient response to treatment. Staining of immune cells versus tumor cells, extracellular versus intracellular staining, and the presence of T cells near the staining may all provide clues about a therapy’s method-of-action as well as how tumors confer resistance to therapies, which may uncover novel targets for treatment.8
While there are many challenges associated with biomarker identification among checkpoint proteins, Louis M. Weiner, MD, director of the Lombardi Comprehensive Cancer Center at Georgetown University in Washington DC, believes that targeting checkpoint proteins will be instrumental in future therapeutics.
“That which makes the cancer survive is also by definition the Achilles heel of the cancer. If you can disable that dominant mechanism, you ought to be able to have a meaningful effect, and I personally think what the whole PD-1/PD-L1 story is about is essentially there are some cancers where this checkpoint is the critical checkpoint,” said Weiner. “I am pretty confident that there are going to be other checkpoints that can be interrogated and used as targets in other diseases.”13
Looking toward the future of melanoma therapy, biomarkers will play instrumental roles in leading decision making for practicing oncologists and their patients, and biomarker identification, validation, and standardization will contribute to improved survival in this cancer patient population.
References
- Robert C, Thomas L, Bondarenko I, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma.N Engl J Med. 2011;364(26):2517-2526.
- Hamid O, Robert C, Daud A, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma.N Engl J Med. 2013;369(2):134-144.
- Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer.N Engl J Med. 2012;366(26):2443-2454.
- Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma.N Engl J Med. 2010;363(8):711-723.
- Hamid O, Dreicer R, Herbst RS, Socinski MA, Weiner LM. Future Role of Checkpoint Inhibitors in Melanoma. OncLive website. http://www.onclive.com/peer-exchange/immunotherapy/Future-Role-of-Checkpoint-Inhibitors-in-Melanoma. Published August 4, 2014. Accessed November 16, 2014.
- Cancer Immunotherapy: Melanoma. Cancer Research Institute website. 2014. http://www.cancerresearch.org/cancer-immunotherapy/impacting-all-cancers/melanoma. Updated August 2014. Accessed November 16, 2014.
- Sznol M. The Promise of PD-1/PD-L1 Antagonists in Treating Metastatic Melanoma. Cancer Therapy Advisor website. http://www.cancertherapyadvisor.com/the-promise-of-pd-1pd-l1-antagonists-in-treating-metastatic-melanoma/article/344658/.2014. Published May 1, 2014. Accessed November 16, 2014.
- Incollingo BF. Herbst Tackles Key Questions in Emerging PD-1/PD-L1 Immunotherapy in NSCLC. OncLive website. http://www.onclive.com/conference-coverage/ilcc-2014/Herbst-Tackles-Key-Questions-in-Emerging-PD-1-PD-L1-Immunotherapy-for-NSCLC. Published August 2, 2014. Accessed November 16, 2014.
- Herbst R. Talk presented at: 14th Annual Targeted Therapies of the Treatment of Lung Cancer Meeting; February 19-22, 2014.
- Prilutskaya M, Pustilnik J, Balukova O, Dyakova N, Fenik L. Quality Bio-Specimens for Novel Biomarker Discovery.Translational Medic. 2012. doi: 10.4172/2161-1025.S1-007.
- Goodman A. Expert Point of View: Mario Sznol, MD. ASCO Post. May 1, 2014. http://www.ascopost.com/issues/may-1,-2014/expert-point-of-view-mario-sznol,-md.aspx. Accessed November 16, 2014.
- Chau CH, Rixe O, McLeod H, Figg WD. Validation of analytic methods for biomarkers used in drug development. Clinical cancer research : an official journal of the American Association for Cancer Research 2008;14(19):5967-5976.
- Weiner LM, Hamid O, Dreicer R, Herbst RS, Socinski MA. Future Role of Immunotherapy in Cancer. OncLive website. http://www.onclive.com/peer-exchange/immunotherapy/Future-Role-of-Immunotherapy-in-Cancer. Published September 8, 2014. Accessed November 19, 2014.