Budding Research Reveals Potential for Prediction of Recurrence in TNBC
“While these findings cannot be exploited to improve clinical decision making today, our results, and the underlying data, collected on an increasingly rare group of triple-negative breast cancer patients treated with locoregional therapy alone, are a valuable contribution to ongoing research on the development, progression and ultimate treatment of triple-negative breast cancer."
A set of molecular markers linked to methylation have been identified, which can potentially predict the risk of cancer recurrence within 5 years for patients with triple-negative breast cancer (TNBC), supporting the standard practice to treat with adjuvant chemotherapy in all patients with TNBC, according to a press release.1
A study conducted from Johns Hopkins University, the University of Iowa, and Duke University confirmed that higher levels of methylation are associated with earlier recurrence and worse outcomes, but the findings did not determine specific levels that could be used to personalize treatment for patients.
High methylation levels appeared to be associated with short recurrence-free intervals in patients who had not received chemotherapy and those who had received chemotherapy (100 marker panel, P =.002; 30 marker panel, P =.05). Among these loci, chromosome 19 sites were enriched.2
“While these findings cannot be exploited to improve clinical decision making today, our results, and the underlying data, collected on an increasingly rare group of TNBC patients treated with locoregional therapy alone, are a valuable contribution to ongoing research on the development, progression and ultimate treatment of TNBC,” wrote the study authors lead by Mary Jo Fackler, PhD, Johns Hopkins University.
The results from this study suggest it may be appropriate to manage patients with less aggressive disease more conservatively while patients with more aggressive disease should be treated earlier. The trial compared 2 different methylated panels of 100 and 30 markers to determine if a subgroup of patients could be identified with better outcomes.
Investigators identified high levels of methylation were associated with poorer outcomes in samples from patients who received locoregional treatment and no chemotherapy in the International Breast Cancer Study Group (IBCSG) trials VIII and IX. The Kaplan-Meier plot demonstrated high tumor methylation led to shorter recurrence-free intervals. However, these results were not statistically significant.
In an analysis of patients who received chemotherapy and locoregional therapy in the IBCSG trials, the higher levels of methylation were again associated with an increased risk of 5-year recurrence, and these results were statistically significant. High methylation was associated with recurrent with the 100-marker panel (Odds ratio [OR] = 1.26; P =.004), but the association was not as strong with the 30-marker panel (OR = 1.30; P=.10).
Patients who consistently benefitted from chemotherapy, which support the current standard of care to administer adjuvant chemotherapy to all patients with TNBC.
Investigators concluded that the adequate characterization of patients with TNBC requires broader molecular signatures. The 30 CpG marker panel had less discriminatory power compared with the 100-marker panel, pointing to the heterogeneity of this disease. The 30 CpG loci were enriched in genes demonstrating DNA binging and transcription regulatory functions. Chromosome 10-specific probes were enriched among both marker sets compared to the array as a whole.
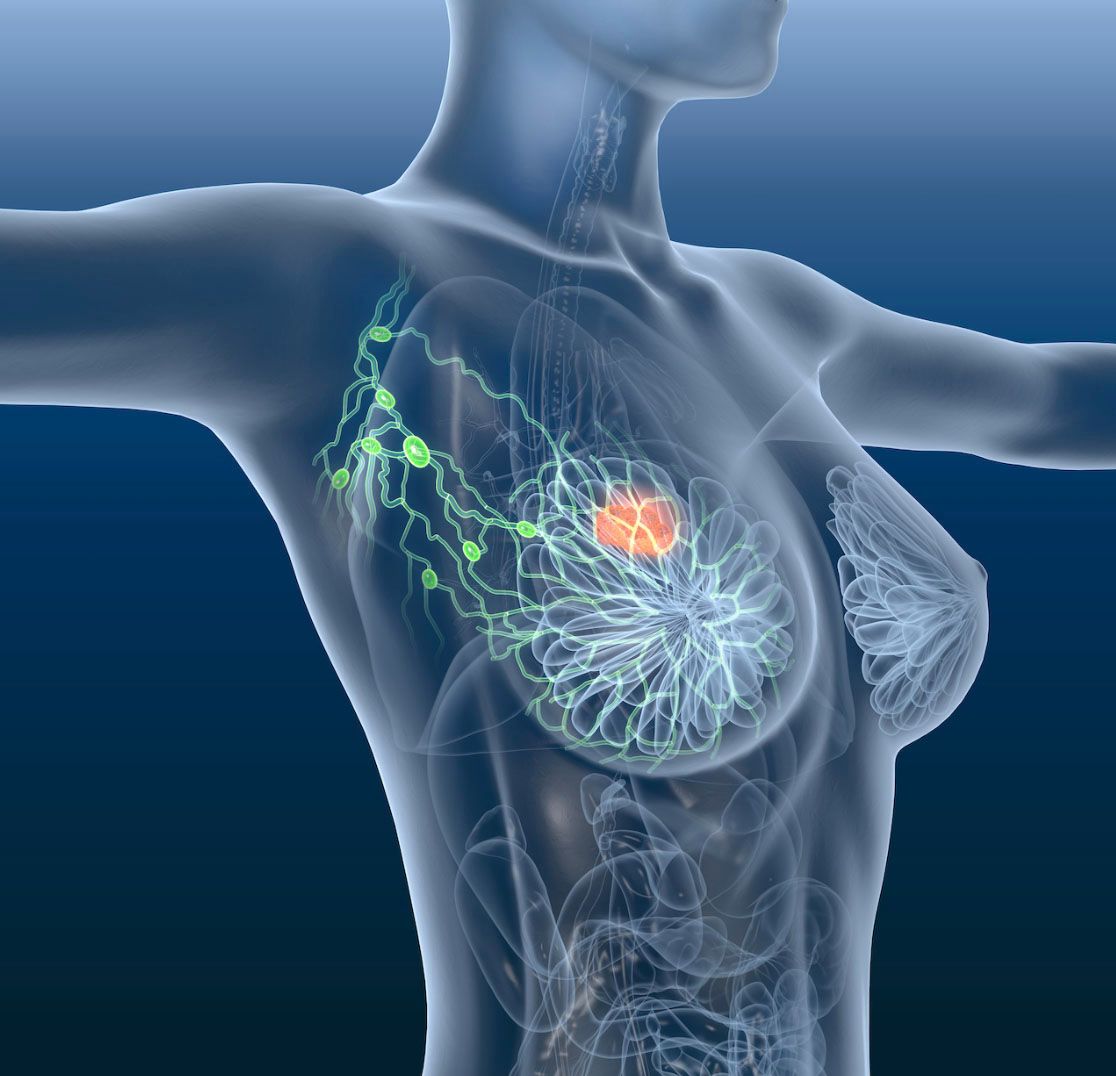
TNBC represents 15% of all breast cancer cases and tend to be more aggressive. Patients with TNBC tend to have poorer outcomes than other types of breast cancer, and these tumors tend to become resistant to therapies targeting hormone receptors for estrogen and progesterone, as well as HER2.
The goal of this study was to develop tools to risk-stratify patients with TNBC to predict recurrence. Breast cancer tissue samples from 110 patients with TNBC were analyzed. Tissue was collected from repositories at the 3 institutions. A methylation array analysis was performed on all of the samples. Discovered marker sets were tested by Kaplan-Meier analyses prospectively on 49 samples in the no-chemotherapy patient population.
“In conclusion, our hypermethylation signatures identify increased recurrence risk independent of whether patients receive chemotherapy,” Fackler et al concluded.
References
- Researchers Identify Molecular Markers That May Help Predict Disease Recurrence Risk for Triple-Negative Breast Cancer Patients [news release]. Johns Hopkins Medicine. May 1, 2020. https://bit.ly/2YEj4JZ. Accessed May 5, 2020.
- Fackler M, Cho S, Cope L., et al. DNA methylation markers predict recurrence-free interval in triple-negative breast cancer. npj Breast Cancer. 2020; 6;(3). https://doi.org/10.1038/s41523-020-0145-3.