BRUIN MCL-321 Trial Evaluates Pirtobrutinb Monotherapy in MCL
In an interview with Targeted Oncology, Michael Wang, MD, discussed the rationale of the phase 3 study and how positive results from this trial may further shape the mantle cell lymphoma treatment landscape.
Michael Wang, MD
Though the addition of covalent Bruton tyrosine kinase (BTK) inhibitors have immensely changed the treatment landscape of relapsed mantle cell lymphoma (MCL), the majority of patients still require additional treatment. As a result, researchers developed pirtobrutinib (Jaypirca), a highly selective, non-covalent BTK inhibitor to address this unmet need.1
Pirtobrutinib was granted FDA approval in January 2023, based on findings from the phase 1/2 BRUIN trial (NCT03740529) which evaluated pirtobrutinib 200 mg once daily in 120 patients with MCL. To further evaluate the benefit of pirtobrutinib in this patient population, the randomized, phase 3 BRUIN MCL-321 trial (NCT04662255) was developed.
This trial is currently assessing treatment with pirtobrutinib vs investigator's choice of a BTK inhibitor, either acalabrutinib (Calquence), or zanubrutinib (Brukinsa) in patients with previously treated, BTKi-naive MCL to determine the superiority of pirtobrutinib in this space.
The global, randomized, open-label, phase 3 study trial is enrolling approximately 500 patients with a diagnosis of MCL who have also received at least 1 line of therapy, have an ECOG performance status of 0-2, have measurable disease by imaging per Lugano criteria, and have progressed on or relapsed following their most recent line of therapy.
Investigators are assessing the primary end point of progression-free survival (PFS) along with the secondary end points of overall response rate, duration of response, investigator-assessed PFS per Lugano criteria, overall survival, event-free survival, time to treatment failure, time to next treatment, PFS2, safety, tolerability, and patient reported outcomes.
In an interview with Targeted OncologyTM, Michael Wang, MD, Puddin Clarke endowed professor of lymphoma and myeloma at The University of Texas MD Anderson Cancer Center, discussed the rationale of the phase 3 study and how positive results from this trial may further shape the MCL treatment landscape.
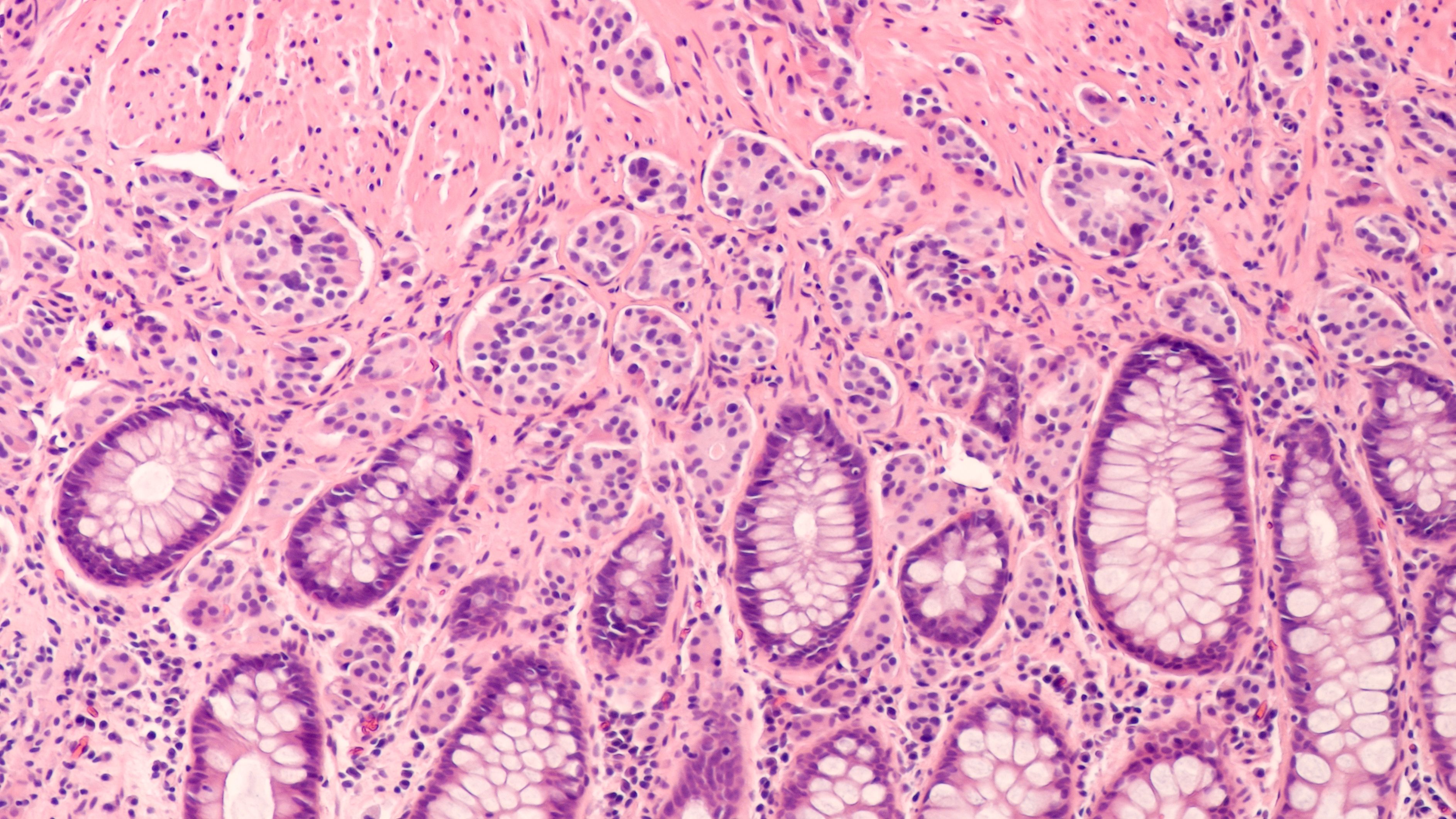
Lymphomas: © David A Litman - stock.adobe.com
Targeted Oncology: Can you discuss the methods and design of the BRUIN MCL-321 trial?
Wang: [This is a] trial in progress, the phase 3 clinical trial with pirtobrutinib. [For] the trial design, this is a phase 3, international trial recruiting 500 patients. There are 2 arms. The experimental arm is the pirtobrutinib monotherapy vs the physicians choice of any covalent BTK inhibitors including acalabrutinib and zanabrutinib. The arm used to include the ibrutinib, and now, the ibrutinib [Imbruvica] has been withdrawn because of the most recent voluntary withdrawal, so there are [now] 2 arms.
The patient population consists of patients with relapsed mantle cell lymphoma. The patient population is 500 international patients. This is a phase 3 clinical trial, randomized, and in a population of patients with mantle cell lymphoma that have not been treated with any BTK inhibitors.
What led to the initiation of this trial?
The reason we want to do it is because the preliminary phase 2 clinical trial showed that pirtobrutinib is really active when you have mantle cell lymphoma. It is even effective after resistance it has developed with a BTK inhibitor in patients with relapsed mantle cell lymphoma. The response rate was very impressive with refractory patients.
Based on the phase 2 clinical trial, the FDA has approved pirtobrutinib for relapsed/refractory mantle cell lymphoma in the [United States]. Based on the phase 2 clinical trial, in order to gain full approval, they designed this a phase 3 trial. In the phase 2 clinical trial, the response rate for pirtobrutinib after a BTK inhibitor was 54%, but in the patients who had not been exposed with a covalent BTK inhibitor, usage of pirtobrutinib caused efficacy of 85%. Therefore, we think that pirtobrutinib without prior BTK inhibitors can be compared with any covalent BTK inhibitor.
Therefore, [that influenced] this phase 3 clinical trial design. If this trial is successful, pirtobrutinib will be used before the covalent BTK inhibitor usage, so this is a very significant clinical trial.
Where do you feel future research of pirtobrutinib will be focused?
I really think that for pirtobrutinib, a phase 3 clinical trial is only the first step. In the meantime, pirtobrutinib’s usage is being explored in combinations, such as in combination with venetoclax, rituximab, and in [other] combinations.
In the future, I think that pirtobrutinib will be studied as maintenance close to chimeric antigen receptor [CAR] T, will be studied after CAR T failures, will be used as a bridging therapy before CAR T, so bispecific antibodies, and it can be combined with not only targeted therapies, but also with immunotherapies such as bispecific or trispecific antibodies or CAR T-cell therapies. [A] phase 3 study is the first step, but other steps are progressing concurrently.
Other major studies, not only at the phase 3, but other smaller studies with investigator-initiated trials are ongoing.
What unmet needs still exist in this space?
There's a huge unmet need when the patient is resistant to covalent BTK inhibitors, and if they have progressed or relapsed, we use CAR T cells because CAR T-cell efficacy is high, but its toxicity is [also] high. So, if the patient had relapsed after BTK inhibitors, they are not high-risk. They have small tumors, and they do not need immediate CAR T-cell therapy. You could put this patient in long-term remission using only pirtobrutinib as shown in the phase 2 clinical trial that has been recently published in the Journal of Clinical Oncology. Other major studies are not only at the phase 3, but other smaller studies with the investigator initiated trials are ongoing.
REFERENCE
Eyre TA, Shah NN, Le Gouill S, et al. P1100: BRUIN MCL-321: A phase 3 open-label, randomized study of pirtobrutinib vs investigator choice of BTK inhibitor in patients with previously treated, BTK inhibitor naïve mcl (trial in progress). Hemasphere. 2022;6(Suppl ):990-991. Published 2022 Jun 23. doi:10.1097/01.HS9.0000847268.67095.fc
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More