brPROPHET May Better Detect ctDNA and Identify MRD in Colorectal Cancer
According to initial data presented at the 2023 Gastrointestinal Cancers Symposium, the novel, personalized, tumor-informed brPROPHET technology was more sensitive in detecting molecular residual disease vs other assays.
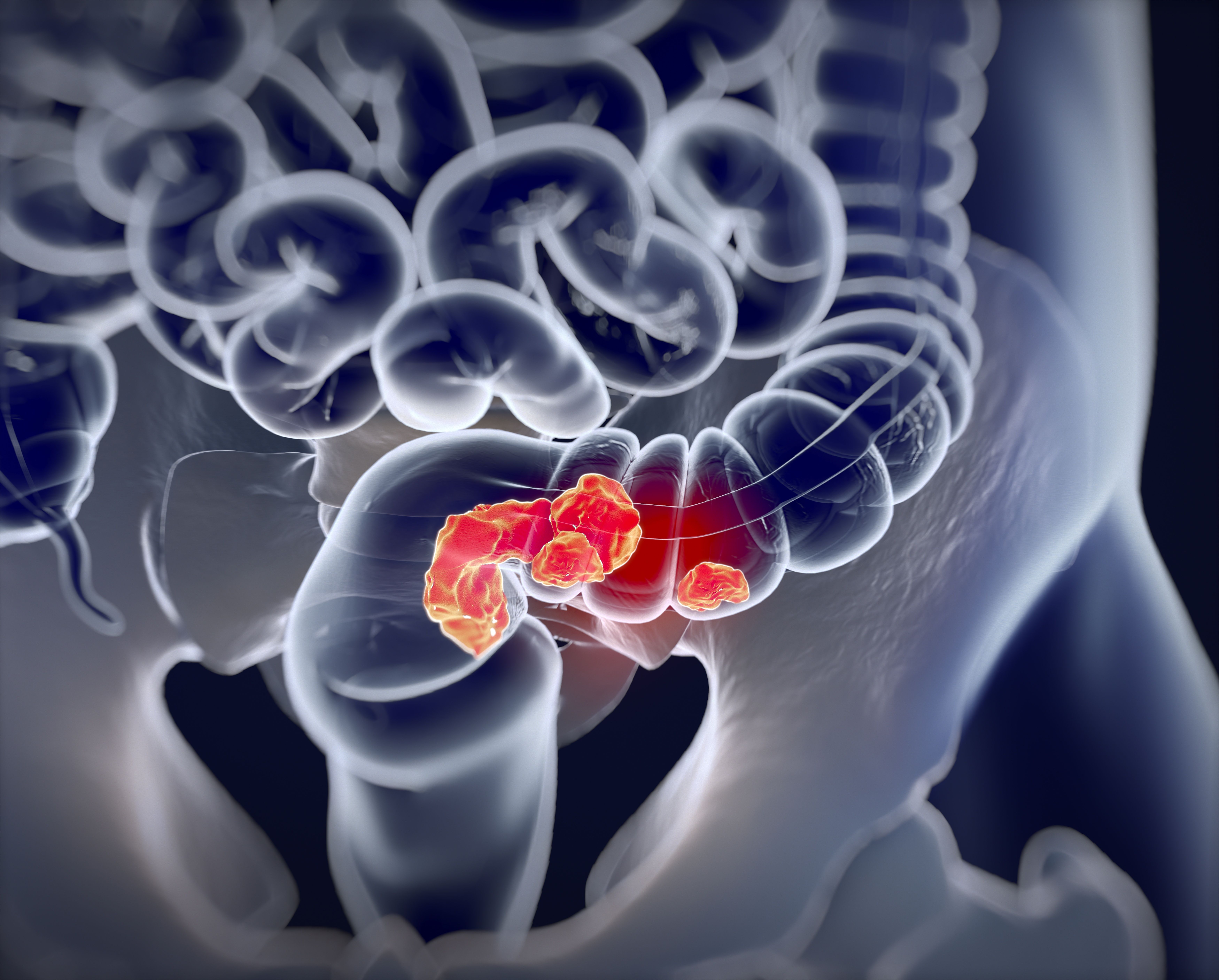
Detecting circulating tumor DNA (ctDNA) and identifying molecular residual disease (MRD) in patients with colorectal cancer (CRC) after surgery was assessed with greater sensitivity using the novel patient-specific prognostic and potential therapeutic marker tracking (brPROPHET) approach when compared with alternatives, according to findings presented at the 2023 Gastrointestinal Cancers Symposium.
The brPROPHET approach detected ctDNA in 97.3% of the 74 patients enrolled for all 3 MRD assays, a higher value than investigators achieved with the fixed panel with informed calling (FI) assay (75.7%) and the fixed panel with agnostic calling (FA) assay (68.9%). This novel technology was also the only assay to capture baseline ctDNA in 15 of these patients (20.3%), who had lower median ctDNA levels (0.3 mean tumor molecules [MTM] / mL) than those captured by FI and FA fixed panels (3.0 MTM/mL; P < .05).
Across 135 postoperative blood samples tested by all 3 assays, brPROPHET achieved a positive rate of 14.8%, as compared with 8.1% and 6.7% achieved by the FI and FA fixed panel assays, respectively.
“This method [brPROPHET] was developed to detect MRD with a limit of detection of 0.004% and a sample level specificity of over 99% in the analytical validation,” presenting author Di Cao, MD, a physician at Sun Yat-sen University Cancer Center in Guangzhou, China, said during the presentation. “[Our] study reported that the clinical validation of the brPROPHET assay in colorectal cancer demonstrated superior sensitivity in detecting preoperative and post-operative ctDNA [vs] fixed-panel assays.”
The brPROPHET assay is designed to trace patient-specific somatic variants based on whole-exome sequencing of the tumor tissue and matched white blood cells. It targets up to 55 variants per patient.
The study investigators evaluated assay sensitivities in a population of 117 patients, including 53 (45.0%) with stage II CRC and 41 (35.0%) with stage III. They performed FI and FA fixed panel assays in a subset of patients with a 168-gene panel spanning 273 kilobases of the human genome for comparison with brPROPHET. Sixty (51.0%) patients received adjuvant therapy after surgery.
“Of the designed variants for ctDNA detection, only 6%...were included in the fixed panel. Seventy-five percent of genes selected for panel design were private to a specific patient, suggesting the broadness of MRD detection,” Cao said.
The median patient age of the population was 57 years. Most enrolled patients were male (55.5%), and a plurality had left-sided disease (42.7%) rather than right-sided (26.5%), rectal (23.9%), or transverse (6.8%) disease.
Preoperative ctDNA was detected in 97% of patients (n = 113) overall; much higher detection rates occurred in patients with later stage vs stage I disease. Additionally, median ctDNA levels were higher in patients with later stage disease and correlated with tumor volume.
The overall positivity rate declined to 18% on day 7 following surgery and 15% on day 30.
Two patients relapsed during the short follow-up period; ctDNA was detected prior to radiological relapse in both, with a lead time of 1 and 2 months, respectively.
“Identifying MRD with tailored, tumor-informed, ctDNA-based next-generation sequencing (NGS) assays after curative surgery could facilitate the individualized management of [patients with] resected CRC,” the investigators concluded. “Longitudinal monitoring is ongoing for further analysis of clinical outcomes and serial tests.”