Age, Stage, and Refractory Status in Patients With FL Predict Outcomes
An analysis of Medicare patients with follicular lymphoma revealed which characteristics correlated with overall survival.
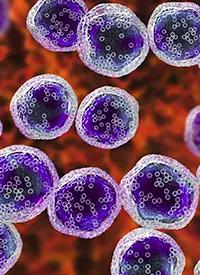
Image credit: © Dr_Microbe - Adobe Stock
Factors such as disease stage, age, and treatment-refractory status are associated with overall survival (OS) in patients with follicular lymphoma (FL), according to a study of over 14,000 real-world patients.1
A study of the SEER- [Surveillance, Epidemiology, and End Results Program]-Medicare database of patients aged 65 and older with FL showed various prognostic factors for worse OS, with double-refractory FL having a 151% higher mortality rate. The results showed patients often receive up to 3 or more lines of therapy, primarily chemoimmunotherapy with an anti-CD20 monoclonal antibody. Very few of these patients received novel therapies such as chimeric antigen receptor (CAR) T-cell therapy.
The analysis identified 14,077 patients diagnosed with FL from January 1, 2000, to December 31, 2017. This only included patients on Medicare who were 65 or older. The median age at diagnosis was 76 years, with a majority of female patients (55.2%) and White patients (94.2%). Forty-five percent had a National Cancer Institute (NCI) Comorbidity Index score between 0 and 1, and 20.4% had a score of 1 or higher. Fifty-two percent had Ann Arbor stage III or IV disease at diagnosis.
Data were available for 8967 patients who received at least 1 line of therapy. Sixty percent received either rituximab (Rituxan) or obinutuzumab (Gazyva) plus chemotherapy in the first line, 31.3% received rituximab or obinutuzumab monotherapy, and 8.5% received chemotherapy alone. Only 44.6% and 41.9% received a combination chemoimmunotherapy in the second and third lines, respectively.
Novel therapies, including CAR T-cell therapy and PI3K inhibitors, were not used by any patients in the first line, 0.4% in the second line, and 1.7% in the third line and later.
The median OS in this population for patients who received first-line therapy was 81.9 months and only 49.6 months in patients who received a second-line therapy. The median OS was 35.1 months, 27.1 months, and 22.6 months in patients who received 3, 4, and 5 lines of therapy, respectively. A sensitivity analysis that excluded patients with ICD-O-3 morphology
9690/3 FL (NOS [not otherwise specified]) and used a no-treatment gap of at least 365 days to define maintenance therapy with an anti-CD20 monoclonal antibody found similar OS outcomes.
Patients were at higher risk of death based on age group at diagnosis. The median OS for patients aged 65 to 70 was 145.4 months. For those 71 to 75 years old, it was 110.4 months, for those 76 to 80, it was 81.1 months, and for those 81 or older, it was 40.5 months. Patients aged 71 to 75, 76 to 80, and 81 and older had increased mortality rates of 35%, 95%, and 248%, respectively, compared with those aged 65 to 70.
Patients diagnosed with later-stage disease also had worse survival outcomes. Median OS for stage I/II was 89.1 months compared with 78.6 months for stage III and 72.1 months for stage IV. Patients diagnosed at stage III and IV had a 26% and 46% increased mortality rate, respectively, when compared with those diagnosed at stage I or II.
Based on a Cox proportional-hazard model adjusting for covariates, analysis showed that patients with double-refractory disease, defined as being refractory to an anti-CD20 antibody and alkylating therapy, had a 151% or higher mortality rate compared with all patients who were not double refractory (adjusted HR, 2.51; 95% CI, 2.29-2.74).
Patients with grade III FL also appeared to have worse OS outcomes than those with grade I or II disease (adjusted HR, 1.16; 95% CI, 1.09-1.23), as did those with unspecified disease grade (adjusted HR, 1.20; 95% CI, 1.15-1.26).
Patients with NCI Comorbidity Index score of between 0 and 1 had an increased risk of mortality than those with a score of 0 (adjusted HR, 1.29; 95% CI, 1.23-1.36). Those with a score of 1 or higher had over twice as great a risk of mortality compared with those with a score of 0 (adjusted HR, 2.16; 95% CI, 2.04-2.29).
These results demonstrate that older patients with FL in the United States have poor outcomes if they have comorbidities including those associated with age. Additionally, it is uncommon for patients to survive long if they do not respond to initial therapies. Outcomes may be different in the greater FL population including younger patients and those who have other healthcare coverage. Additionally, novel therapies such as CAR T-cell therapy, PI3K inhibitors, and bispecific antibodies have become more commercially available, but they may have been available only for fit patients in clinical trials at the time period covered by this dataset.
“These findings underscore the heterogeneity of FL and highlight the need for novel effective therapies,” the study authors concluded in their poster.
REFERENCE
1. Yang S, Bains Chawla S, Zhang G, et al. Real-world treatment patterns and survival among follicular lymphoma patients: A SEER-Medicare analysis. Presented at: International Society for Pharmacoeconomics and Outcomes Research (ISPOR) 2023; May 7-10, 2023; Boston, MA. Accessed May 10, 2023. https://bit.ly/3HYTGVb
Does Odronextamab Show Hope in FL and DLBCL Despite Regulatory Hurdles?
November 5th 2024Despite regulatory challenges from the FDA, odronextamab has received European approval for the treatment of patients with relapsed/refractory follicular lymphoma or diffuse large B-cell lymphoma following 2 prior treatments.
Read More
Phase 3 Trial of Tafasitamab in Follicular Lymphoma Meets Primary End Point
August 16th 2024The phase 3 inMIND trial evaluating tafasitamab in combination with lenalidomide and rituximab in relapsed or refractory follicular lymphoma showed promising progression-free survival findings, according to topline results.
Read More