Adding Vistusertib to Anastrozole Improves Safety and PFS in Patients with Endometrial Cancer
Improvement in progression-free survival and safety demonstrated with the addition of vistusertib to anastrozole vs anastrozole alone in patients with hormone receptor−positive recurrent or metastatic endometrial cancer.
The progression-free rate at 8 weeks (8wk-PFR), overall response rate, and progression-free survival (PFS) rate all improved when the mTOR inhibitor, vistusertib (AZ-2014), was added to anastrozole (Arimidex) treatment compared with anastrozole alone in patients with hormone receptor−positive recurrent or metastatic endometrial cancer in the VICTORIA study (NCT02730923).1
The combination arm (n = 49) had an 8wk-PFR of 67.3% (unilateral 95%CI, 54.7%), and the anastrozole alone arm (n = 24) had an 8wk-PFR of 39.1% (unilateral 95% CI, 22.2%). Investigators also found no significant serious adverse events (SAEs) during the safety run-in period.
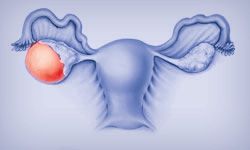
Endometrial cancer is often hormone-dependent and treated with aromatase inhibitors. The PI3K-AKT-mTOR pathway deregulation found in endometrial cancers drives hormonal resistance, supporting the rationale for investigators to combine this mTOR inhibitor with endocrine therapy.
The VICTORIA trial is a multicenter open-label phase 1/2 randomized clinical trial. The study enrolled 75 women with hormone receptor−positive recurrent or metastatic endometrial cancer across 12 cancer centers in France from April 2016 to October 2019, and 73 patients were randomized 2:1 to receive 125 mg of oral vistusertib twice daily for 2 days per week plus 1 mg of oral anastrozole daily or oral anastrozole alone. Data analyses were performed from December 11, 2020, to March 11, 2021. The study incorporated a safety run-in period, and a Simon 2-stage design was used.
The primary end points were SAEs for the safety run-in period and 8wk-PFR, which was assessed by blinded independent central review in phase 2 of the study. Secondary end points included objective response rate, duration of response, PFS, overall survival, and incidence of AEs.
Patients in the vistusertib plus anastrozole arm had an overall response rate of24.5% (95% CI, 13.3%-38.9%) compared with 17.4% (95% CI, 5.0%-38.8%) in the anastrozole-alone arm. At a median follow-up of 27.7 months, the median PFS for the combination arm was 5.2 (95% CI, 3.4-8.9) vs 1.9 months (95% CI, 1.6-8.9) months in the control arm.
The median age of patients was 69.5 years (range, 37-88). Approximately half of patients in the combination arm had ECOG performance scores of 0 (53%) and the other half 1 (47%), whereas 38% of patients scored 0 and 63% scored 1 in the anastrozole-alone arm. About 80% of patients in both arms had FIGO stage IV, and the rest had stage III. The most frequent histologic subtype was endometroid across both arms, as reported in the combination arm (88%) and in the control arm (79%). Fifty-five percent of patients in the vistusertib plus anastrozole arm had 1 prior chemotherapy treatment and 58% of patients in the anastrozole arm had 1 prior chemotherapy treatment; the rest of the patients had no prior chemotherapy.
The most common any grade AEs in patients receiving vistusertib and anastrozole were nausea (51%), fatigue (69%), and diarrhea (41%). Fatigue, lymphopenia, hyperglycemia, and diarrhea were the most common grade 2 or higher AEs associated with vistusertib. The most common any grade AEs in the control arm were similar to the experimental arm: fatigue (29%), arthralgia (29%), and diarrhea (13%). Investigators reported 3 SAEs in the anastrozole alone arm.
These safety and efficacy data demonstrate clinically meaningful improvement with a manageable safety profile for patients with recurrent or metastatic endometrial cancer. Investigators suggest further research on the selection of patients with endometrial cancer for endocrine therapy. Specifically, identifying molecular subgroups would allow for more precise patient selection who may experience more favorable outcomes.
References
Heudel P, Frenel JS, Dalban C, et al. Safety and efficacy of the mTOR inhibitor, vistusertib, combined with anastrozole in patients with hormone receptor-positive recurrent or metastatic endometrial cancer: the VICTORIA multicenter, open-label, phase 1/2 randomized clinical trial. Published online May 12, 2022. JAMA Oncol. 2022;e221047. doi:10.1001/jamaoncol.2022.1047
Lenvatinib-Pembrolizumab Duo Delivers Impressive Results in Endometrial Cancer
September 18th 2024The combination of lenvatinib and pembrolizumab showed promising results in treating recurrent endometrial carcinoma, demonstrating significant antitumor activity and improved survival rates compared to standard therapy.
Read More