Second-Line Cemiplimab Improves Survival and Quality of Life in Cervical Squamous Cell Carcinoma
Results from the EMPOWER-Cervical 1/ GOG-3016/ENGOT-cx9 trial led the FDA to grant priority review to cemiplimab as treatment of patients with recurrent or metastatic cervical cancer whose disease progressed on or after chemotherapy.
Krishnansu S. Tewari, MD

Cemiplimab (Libtayo) reduced the risk of death by 27% vs chemotherapy in patients with recurrent and metastatic cervical squamous cell carcinoma following progression on first-line platinum-containing chemotherapy, according to results of the phase 3 EMPOWER-Cervical 1/ GOG-3016/ENGOT-cx9 trial (NCT03257267).
“In the largest randomized study conducted to date in this population, cemiplimab is the first immunotherapy to demonstrate a statistically significant and clinically meaningful survival benefit in recurrent/metastatic cervical carcinoma following progression after first-line platinum- containing chemotherapy,” said Krishnansu S. Tewari, MD, when presenting the findings during the 2021 International Gynecologic Cancer Society Annual Global Meeting. “Cemiplimab can provide a new standard-of-care treatment option for this population, which has been associated with a very poor prognosis,” he added.
Following results of the trial, the FDA granted a priority review to cemiplimab as treatment of patients with recurrent or metastatic cervical cancer whose disease progressed on or after chemotherapy.2
The open-label, randomized trial enrolled 608 patients with recurrent and metastatic cervical cancer resistant to platinum-based chemotherapy to be treated in second-line setting or beyond with cemiplimab or chemotherapy.
Patients were randomized to receive intravenous cemiplimab 350 mg every 3 weeks or investigator’s choice of chemotherapy given for up to 96 weeks. Chemotherapy options included pemetrexed, gemcitabine, topotecan, irinotecan, and vinorelbine.
Two interim analyses were prespecified in the study protocol. At the first interim analysis, the Independent Data Monitoring Committee (IDMC) recommended the trial continue. At the second interim analysis, the IDMC recommended that the trial be stopped early for efficacy. Statistically, OS was looked at first in patients with squamous cell carcinoma and then in the overall population.
The median age was 51 (range, 22-87) and the majority of patients had an ECOG performance status of 1 (53.5%), metastatic disease (94.4%), and only 1 prior line of therapy for recurrent/metastatic disease (56.9%). Squamous cell carcinoma histology accounted for the majority of patients (77.8%), 19.1% had adenocarcinoma, and 3.1% had adenosquamous carcinoma. Less than half of all patients (n = 254) had baseline PD-L1 expression samples.
At a median follow-up of 16.8 months (range, 6.0-38.2), the median OS in the squamous cell carcinoma group was 11.1 months (95% CI, 9.2-13.4) with cemiplimab in comparison with 8.8 months (95% CI, 7.6-9.8) with chemotherapy (HR, 0.73; 95% CI, 0.58-0.91; one-sided P = .00306).
“In this first step of the hierarchical analysis, the superiority of cemiplimab over chemotherapy in improving overall survival is apparent and significant in this population of squamous cell carcinoma,” said Tewari, The Philip J. DiSaia, MD, Chair in Gynecologic Oncology, Obstetrics, and Gynecology, UCI School of Medicine in Orange, California.
The OS for the overall population was 12.0 months (95% CI, 10.3-13.5) in the cemiplimab-treated patients compared with 8.5 months (95% CI, 7.5-9.6) in the chemotherapy-treated patients (HR, 0.69; 95% CI, 0.56-0.84; one-sided P = .00011). In the adenocarcinoma population, the median follow-up was 21.9 months (range, 6.9-36.6), at which point the median OS was 13.3 months (95% CI, 9.6-17.6) with cemiplimab vs 7.0 months (95% CI, 5.1-9.7) with chemotherapy (HR, 0.56; 95% CI, 0.36-0.85; one-sided P < .005).
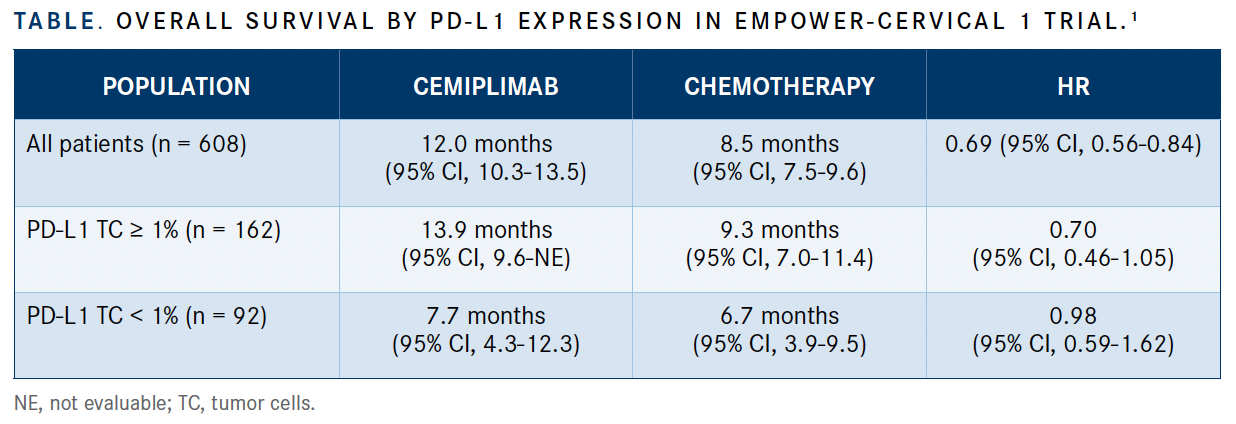
Benefit for cemiplimab therapy was observed across all prespecified subgroups in terms of OS. Patients treated with cemiplimab who had positive PD-L1 expression on tumor cells benefited the most (median OS, 13.9 months) in comparison with those with negative PD-L1 expression (7.7 months) and those treated with chemotherapy (9.3 months with positive PD-L1 expression, 6.7 months with negative expression) (TABLE).
PFS was similar between the 2 arms; the median was 2.8 months (95% CI, 2.6-3.9) in the cemiplimab arm vs 2.9 months (95% CI, 2.7-3.4) in the chemotherapy arm (HR, 0.75; 95% CI, 0.63-0.89). Median PFS was similar in patients with positive PD-L1 expression; however, patients with negative PD-L1 expression in the cemiplimab arm had a median PFS of 1.9 months (95% CI, 1.4-4.0) vs 2.9 months (95% CI, 2.0-4.2) in the chemotherapy arm (HR, 1.00; 95% CI, 0.62-1.60).
ORR was 16.4% (95% CI, 12.5%-21.1%) in the cemiplimab arm vs 6.3% (95% CI, 3.8%-9.6%) with chemotherapy (odds ratio, 2.98; 95% CI, 1.71-5.22). In patients with measurable PD-L1 expression, the ORR was 18.3% (95% CI, 10.6%- 28.4%) in those with positive expression and 11.4% (95% CI, 3.8%-24.6%) in those with negative expression among the cemiplimab-treated group. With chemotherapy treatment, patients with positive expression had an ORR of 7.5% (95% CI, 2.8%-15.6%) and 8.3% (95% CI, 2.3%- 20.0%) with negative expression.
No new safety signals were observed in this analysis. Overall, any-grade treatment-emergent adverse events (TEAEs) were reported in 88.3% of patients treated with cemiplimab and in 91.4% of chemotherapy-treated patients; grade 3-5 TEAEs were reported in 45.0% and 53.4% of patients in the cemiplimab and chemotherapy arms, respectively.
Overall rates of TEAEs were lower in the cemiplimab arm in terms of anemia (35.0% vs 44.5% with chemotherapy), nausea (18.3% vs 33.4%, respectively), and vomiting (16.0% vs 23.4%). TEAEs led to discontinuation in 8.7% of patients in the cemiplimab arm and in 5.2% of patients in the chemotherapy arm.
REFERENCE:
1. Tewari KS, Monk BJ, Vergote I, et al. EMPOWER-Cervical 1/GOG-3016/ENGOT-cx9: Results of phase 3 trial of cemiplimab vs investigator’s choice (IC) chemotherapy (chemo) in recurrent/metastatic (R/M) cervical carcinoma. Presented at: 2021 International Gynecologic Cancer Society Annual Global Meeting; August 30-September 2, 2021; Rome, Italy + Virtual.
2. FDA accepts Libtayo (cemiplimab-rwlc) for priority review for advanced cervical cancer. News release. Regeneron Pharmaceuticals. September 28, 2021. Accessed September 28, 2021. https://bit.ly/3kMaSC8

Brown Examines Lenvatinib/Pembrolizumab Combination in pMMR Endometrial Cancer
May 17th 2024During a Case-Based Roundtable® event, Jubilee Brown, MD, discussed the efficacy and safety data from the KEYNOTE-775/Study 309 trial of lenvatinib plus pembrolizumab in patients with mismatch repair proficient advanced endometrial cancer.
Read More