Multiple Studies Provide Efficacy Results for Lenvatinib in Thyroid Cancer
Matthew Taylor, MD, reviewed the clinical trials supporting levantinib as a treatment option for a patient with thyroid cancer and discussed the option with a group of oncologists during a Targeted Oncology Case Base Peer Perspectives event.
Matthew Taylor, MD

Matthew Taylor, MD, codirector, Providence Melanoma Program, Providence Cancer Institute, Earle A. Chiles Research Institute, reviewed the clinical trials supporting levantinib as a treatment option for a patient with thyroid cancer. Taylor discussed the option with a group of oncologists during a Targeted Oncology Case Base Peer Perspectives event.
Targeted Oncology™: How do you assuage patient’s fears when they are first referred to an oncologist?
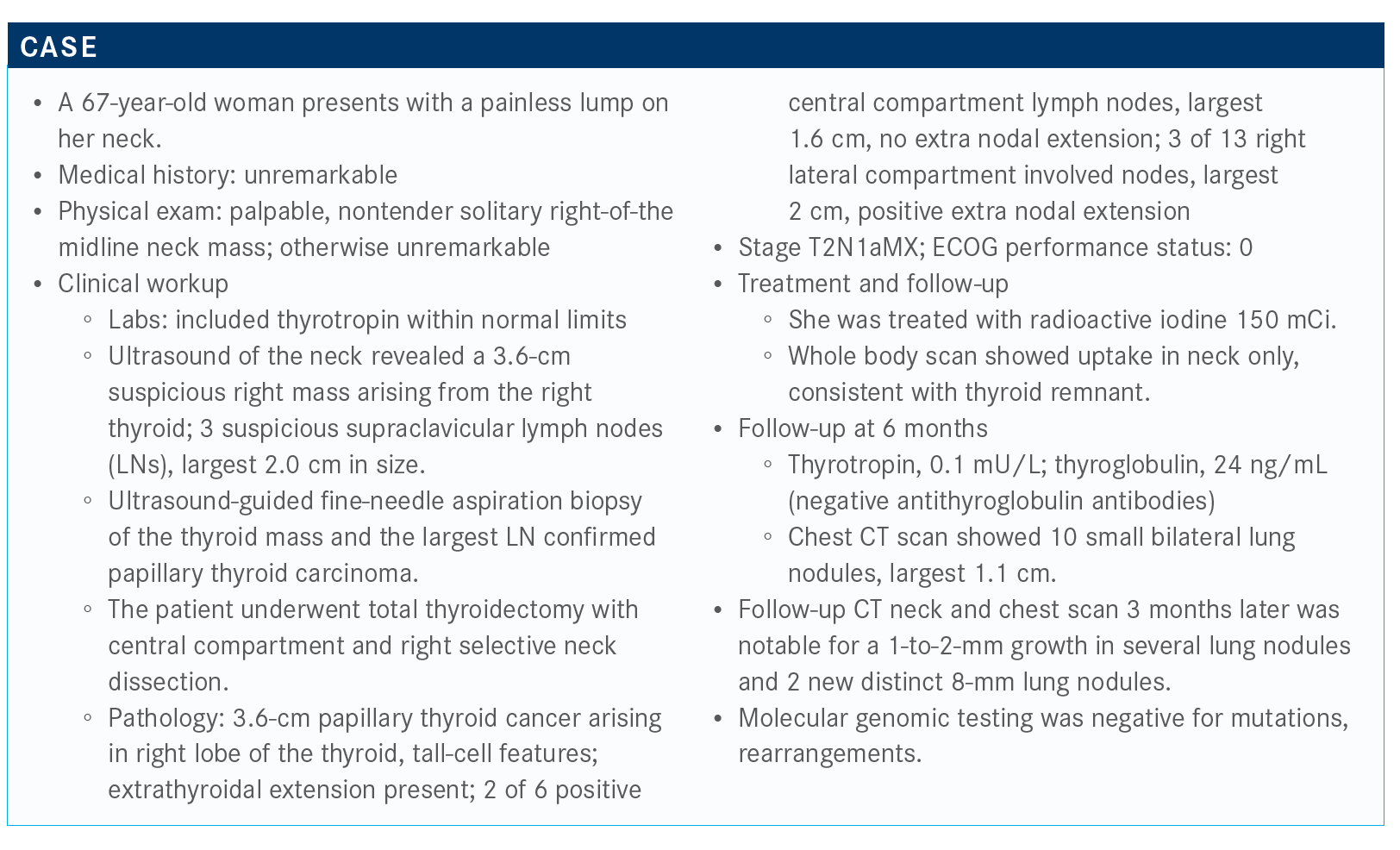
TAYLOR: What I’ve tried to do is work with our endocrinologists to ask that when they send a patient to me that they emphasize that this is an open dialogue to discuss the treatment options. Some patients may have preconceived notions about the medications we use to treat thyroid cancer. Many patients are concerned that they will need to be treated with traditional chemotherapy.
How have the National Comprehensive Cancer Network (NCCN) guidelines evolved in the last decade?
It’s been quite remarkable over the [last] decade to see [the guidelines] grow from what previously [were] nonexistent treatments; now we have a number of drugs that are available as options.1 Lenvatinib [Lenvima] and sorafenib [Nexavar] are preferred systemic therapies. If the patient has an NTRK fusion, then there’s larotrectinib [Vitrakvi] or entrectinib [Rozlytrek]. We’re going to talk about selpercatinib [Retevmo]. Then, of course, if they are TMB [tumor mutation burden] high or MSI [microsatellite instability] high, they’re candidates for immune checkpoint inhibitors.
Please provide an overview of the DECISION trial (NCT00984282) in patients who were refractory to radioiodine.
The DECISION study evaluated patients with radioiodine refractory disease, and, of note, these patients were not allowed to have had prior therapy in the systemic setting.2 Patients were randomized 1:1 to receive either sorafenib or placebo.
One thing I’ll point out, these patients had to show disease progression within 14 months prior to randomization. Some of these patients can have indolent, slow-growing disease. The primary end point was progression-free survival [PFS].
Sorafenib showed a median PFS of a little over 10 months compared with almost 6 months in the placebo arm. The response rate, however, was rather disappointing. The objective response rate [ORR] was only 12% with sorafenib, but that was statistically significant.
As far as safety tolerability, the trial showed a fairly substantial number of patients who had to have some dosing interruption, including dose reductions due to adverse events [AEs]. Almost 19% had to withdraw from treatment due to AEs of the medication.2
Regarding treatment-related AEs, the most common observed in the trial [were] hand-foot syndrome and the typical VEGF receptor inhibitor AEs of diarrhea, hypertension, proteinuria, and fatigue. This is fairly typical for this class of agent.
What are the details of the SELECT trial?
The SELECT trial [NCT01321554] was conducted early in my tenure at Oregon Health & Science University and evaluated lenvatinib, a relatively newer multikinase inhibitor.3 This clinical trial had a similar population as the DECISION trial. Patients had to have cancer that was progressing rapidly—rapidly for thyroid cancer, I should say. They were allowed to have had 1 prior line of therapy and still join the trial. These patients were randomized 2:1 lenvatinib versus placebo. The starting dose of lenvatinib was 24 mg.
When looking at the primary end point of PFS, progression curves separate dramatically. The median PFS with lenvatinib was about 18 months compared with just 3 months in the placebo arm [HR, 0.24; 99% CI, 0.17-0.35; P < .0001]. This cohort was a bit more advanced [in their disease stage] than what we saw in the DECISION trial based on the PFS of the placebo arms, but there is impressive durability of response in these patients.3
The waterfall plot in the study was shockingly impressive because almost all patients treated with lenvatinib had some degree of tumor reduction.
The ORR also was impressive, nearly 65%. The vast majority of patients were partial responders. Again, it’s compelling that so many patients experienced regression of their tumors.
What are the safety profile and toxicities for lenvatinib?
The safety [profile] is similar to the AEs observed with sorafenib and other multikinase inhibitors. Almost everybody had some degree of [adverse] effects in this clinical trial. A high percentage, 76%, had grade 3 toxicity. A significant number of patients experienced significant toxicity.
Remember with sorafenib in the DECISION trial that the discontinuation rate was about 19%; in the lenvatinib study it was about 14%. It’s similar between the 2 trials. Both of these drugs have significant AEs and require a lot of dose reductions to find a tolerable range.
The AE profile is typical of a potent VEGF receptor inhibitor: hypertension, fatigue, diarrhea, and nausea. We do see some hand-foot syndrome with lenvatinib but not nearly as much as with sorafenib. The hypertension is typically more severe with lenvatinib than with sorafenib. I think that really just speaks to the extreme potency of VEGF receptor inhibition.
How does the patient’s age affect PFS?
There [were] some newer data reported from a subgroup analysis [NCT03573960] by Dr. Brose and colleagues.4 This was a prespecified analysis that stratified the patients by age. Basically age 65 years was the cutoff . We saw PFS in both patients [who were elderly] as well as those under the age of 65.
For patients [under] 65 years of age, the median PFS was 20.2 months in the lenvatinib arm versus 3.2 months for the placebo arm [HR, 0.19; 95% CI, 0.13-0.27; P < .001]. In patients [older than] 65, the median PFS in the lenvatinib arm was 16.7 months versus 3.7 months in the placebo arm [HR, 0.27; 95% CI, 0.17-0.43; P < .001].
Does the size of the lung metastases affect outcome, or does it affect your decisions regarding starting treatment?
That’s a great point, and I don’t think anyone knows the answer for sure. At ESMO [European Society for Medical Oncology] 2019, a subgroup analysis looked at the largest size of the patient’s lung metastases, whether it was larger than a centimeter or 1.5 to 2 centimeters. The outcome from this analysis shows that there was still a progression-free and overall survival benefit regardless if the lung metastases were 1 cm, 2 cm, or even larger than that.5
The data suggested that we can start treatment when the tumors are at a smaller size. At 1 cm, patients still have a PFS and overall survival benefit. We don’t have to wait until [the disease has progressed further], then offer the treatment.
If the pace of [disease] progression is rapid and the tumor is growing quickly, it might be a reasonable time to start systemic therapy, even if the tumor is not large enough to cause bleeding and obstruction. We can still prevent the tumor from getting to that point.
Is the 24-mg starting dose of lenvatinib the optimal dose recommended?
There was a clinical trial that we conducted in which we tested the starting dose of 24 mg versus 18 mg for these patients. This was called the Eisai 211 study [NCT02702388].6 The question was if we start at 18 mg, do we get the equivalent benefit [as] if we started at 24 mg?
What we found in the trial was that the response rate was lower and the PFS was lower in the 18-mg cohort than in the 24-mg cohort. That was honestly surprising to me. I didn’t think we were going to see that. I really expected that the 18 mg [dose] would be just as good and certainly better tolerated than the 24-mg [dose].
If my patients are fit enough and healthy enough that I feel [as though] they could potentially tolerate it, I like to start at the 24 mg dose level knowing that quickly we’re going to likely have to undergo some significant dose reductions due to AEs. It seems that when starting patients at that higher dose, you get a significant initial shock to the tumors that results in quick responses. Then, from that point I reduce the dose if needed to manage AEs.
Some patients from the original [SELECT] trial that we started at 24 mg are now down to 10 mg. I even have some patients who are on 4 mg a day, and they’ve been on that dose for years. I do feel [as though] there’s benefit to starting high and then working down to a manageable, tolerable dose. That’s my practice.
References:
1. NCCN. Clinical Practice Guidelines in Oncology. Thyroid carcinoma, version 2.2020. Accessed October 29, 2020. https://bit.ly/2TCNGIq
2. Brose MS, Nutting CM, Jarzab B, et al. Sorafenib in radioactive iodine-refractory, locally advanced or metastatic diff erentiated thyroid cancer: a randomised, double-blind, phase 3 trial. Lancet. 2014;384(9940):319-328. doi:10.1016/S0140-6736(14)60421-9
3. Schlumberger M, Tahara M, Wirth LJ, et al. Lenvatinib versus placebo in radioiodine-refractory thyroid cancer. N Engl J Med. 2015;372(7):621-630. doi:10.1056/NEJMoa1406470
4. Brose MS, Worden FP, Newbold KL, Guo M, Hurria A. Eff ect of age on the efficacy and safety of lenvatinib in radioiodine-refractory differentiated thyroid cancer in the phase III SELECT trial. J Clin Oncol. 2017;35(23):2692-2699. doi:10.1200/JCO.2016.71.6472
5. Tahara M, Kiyota N, Hoff AO, et al. Impact of lung metastasis on overall survival (OS) in the phase 3 SELECT study with lenvatinib (LEN) in patients (pts) with radioiodine refractory differentiated thyroid cancer (RR-DTC). Ann Oncol. 2019;30(suppl 5):v756-v759. doi:10.1093/annonc/mdz267
6. Eisai announces topline results from Study 211 supporting 24 mg as the appropriate starting dose for Lenvima (lenvatinib) in patients with differentiated thyroid cancer. News release. Eisai, Inc; August 11, 2020. Accessed October 29, 2020. https://bit.ly/3ixG6Jn

Anticipating Novel Options for the RAI-Refractory DTC Armamentarium
May 15th 2023In season 4, episode 6 of Targeted Talks, Warren Swegal, MD, takes a multidisciplinary look at the RAI-refractory differentiated thyroid cancer treatment landscape, including the research behind 2 promising systemic therapy options.
Listen
Addressing Informative Censoring Bias in Clinical Trials
November 7th 2024Oncology trials often celebrate treatments improving progression-free survival, yet toxicity-related censoring can bias results. Emphasizing overall survival and quality of life offers clearer insights into true clinical benefit.
Read More