Phase III Nivolumab Study Stopped Early Based on OS Benefit
Frontline treatment with the anti-PD-1 agent nivolumab significantly extended overall survival (OS) when compared with dacarbazine for patients with metastatic or unresectable melanoma.
Melanoma
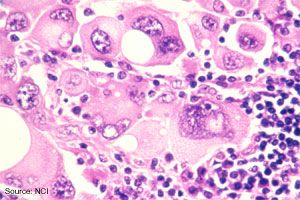
Source: The Web site of the National Cancer Institute (http://www.cancer.gov).
Frontline treatment with the anti-PD-1 agent nivolumab significantly extended overall survival (OS) when compared with dacarbazine for patients with metastatic or unresectable melanoma, according to early phase III results released by Bristol-Myers Squibb (BMS), the company developing the drug.
The randomized trial, labeled CheckMate-066, investigated nivolumab as a treatment for patients with previously untreated BRAF wild-type unresectable stage III and IV melanoma. Following the demonstration of an improvement in survival at the interim analysis, BMS made the decision to unblind the study and allow patients in the dacarbazine arm to cross over.
In the phase III study, 418 patients were randomized in a 1:1 ratio to receive intravenous nivolumab at 3 mg/kg every two weeks or dacarbazine at 1000 mg/m2IV every three weeks. Patients in the study were stratified by PD-L1 status and stage, with PD-L1 defined as ≥5% total membrane staining in tumor cells. Allowing for pseudoprogression commonly seen with checkpoint inhibitors, the study allowed investigators to continue treatment beyond initial progression in patients showing clinical benefit and tolerating therapy.
The primary endpoint of the study was OS, with secondary endpoints focused on progression-free survival, objective response rate (ORR), quality of life, and whether PD-L1 expression was an effective predictive biomarker for OS. Full results are planned for future presentation and publication.
The study was primarily conducted in locations where dacarbazine remains a standard frontline therapy for patients with advanced melanoma, such as Canada. First-line dacarbazine elicits an ORR of 13% and a median OS ranging from 5.6 to 11 months.
A long-term survival update from a phase I study presented at the 2014 ASCO Annual Meeting demonstrated a 3-year OS rate with single-agent nivolumab of 41%. This study examined nivolumab in 107 ipilimumab-naive patients with previously treated advanced melanoma. The ORR was 32% with median response duration of 22.9 months.
In results published earlier this year in theJournal of Clinical Oncologyfrom the phase I analysis, the median OS in nivolumab-treated patients was 16.8 months, and 1- and 2-year survival rates were 62% and 43%, respectively.
In another long-term follow-up presented at the 2014 ASCO Annual Meeting, the combination of nivolumab and ipilimumab nearly doubled median OS compared with either agent alone. The 1- and 2-year OS rates were 85% and 79% with the combination, respectively. Additionally, a preliminary ORR of 43% was reported for 41 patients enrolled to a cohort utilizing a phase II/III dosing regimen of nivolumab monotherapy at 3 mg/kg every 2 weeks.
“The outcome of CheckMate-066 is an important milestone in the field of immuno-oncology as it represents the first well-controlled, randomized phase III trial of an investigational PD-1 checkpoint inhibitor to demonstrate an overall survival benefit,” Michael Giordano, MD, Head of Oncology Development at BMS, said in a press release. “Bristol-Myers Squibb is committed to continuing to lead advances in immuno-oncology and to executing our strategy to provide patients with the best opportunity to achieve the potential for long term survival.”
Nivolumab is currently being explored as a monotherapy and in combination across a variety of tumor types. To date, according to BMS, more than 7,000 patients are receiving treatment with nivolumab in a clinical trial.