Melanoma Therapies in the Pipeline
There are currently numerous experimental therapeutic options in various phases of clinical development that may hold promise for patients with advanced melanoma.
Figure. Mechanism of Action of PD-1 Inhibitors
Mechanism of Action of PD-1 Inhibitors
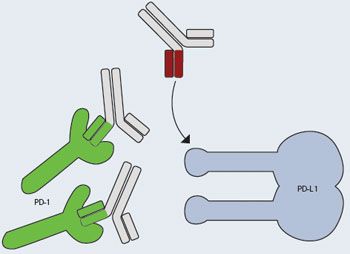
By binding PD-1 on the surface of T cells, cancer cells can evade the immune system. Therapies that block PD-1/PD-L1 can reactivate the immune system.
Small Molecules
MEK Inhibitors
There are currently numerous experimental therapeutic options in various phases of clinical development that may hold promise for patients with advanced melanoma.In the MAPK pathway, MEK kinases are situated immediately downstream of the BRAF kinase; once activated, they trigger activation of pathways responsible for tumorigenesis. GSK1120212 is one such small molecule that has now reached phase III trials for the treatment of melanoma. In a phase III study, this selective, allosteric inhibitor of MEK 1 and 2 induced an objective response in 22% of patients, and 74% experienced some degree of tumor regression. Most common adverse events included diarrhea, rash, and peripheral edema. No cases of SCC occurred.1
Tyrosine Kinase Inhibitor
Nab-paclitaxel
Biologics
Immunotherapy
AZD6244 is another MEK inhibitor that selectively binds to MEK 1 and 2. This drug remains in phase II clinical trials to evaluate its efficacy in treating patients with stage III or IV melanoma.2Lenvatinib is an oral, multitargeted receptor tyrosine kinase inhibitor targeting VEGFR1-3, FGFR1-4, RET, KIT, and PDGFR. In a recent phase II study in which lenvatinib was administered to 93 patients with advanced BRAF wild-type melanoma, some clinical benefits were seen, with confirmed partial responses in 9% of patients, and a 32% clinical benefit rate. Median PFS was 3.7 months, and median OS was 9.5 months. Dose reduction was required to manage toxicity in 46% of patients. Most frequent adverse events included hypertension, fatigue, nausea, diarrhea, and reduced appetite.3Nab-paclitaxel (Abraxane) is a nanoparticle formulation of paclitaxel bound to albumin for injectable suspension. In a randomized, international phase III study in chemotherapy-naïve patients with metastatic melanoma,nab-paclitaxel significantly improved PFS compared with patients receiving DTIC chemotherapy.4Darleukin is a fully human vascular targeting immunocytokine, a fusion protein containing interleukin- 2 (IL-2), which increases the safety of administration of IL-2, and improves its antitumor activity. Darleukin is currently being tested in a randomized, phase IIb study of its efficacy in combination with DTIC, compared with DTIC monotherapy, in patients with metastatic melanoma.1
Allovectin-7 is a plasmid-based immunotherapy expressing HLA-B7 and 2 microglobulin genes, and is designed to stimulate local and systemic antitumor responses. In a phase II single-arm study to evaluate the efficacy of intralesional injection of Allovectin-7 in 127 patients, the overall response rate was 11.8% and median OS was 18.8 months. The median duration of response was 13.8 months, and all responses lasted for more than 6 months.5A phase III trial remains ongoing to compare the safety and efficacy of Allovectin-7 vs DTIC or temozolomide in patients with recurrent stage 3 or stage 4 melanoma.6Patients in the phase II study with similar characteristics to those in the new phase III study (chemo-naïve with a single lesion injected) had a 17% overall response rate, and a median OS of 22.5 months.5
Data have demonstrated clinical benefit of cancer vaccines containing a specific cancer antigen, and a peptide vaccine for melanoma. Toll-like receptor (TLR) agonists have the potential to enhance antitumor T-cell responses, either in combination with incomplete Freund’s adjuvant (IFA) or alone. CD40 ligation at the vaccine site microenvironment may also enhance adjuvant activity. A clinical trial is recruiting patients with resected stage 2B-4 melanoma, and is designed to evaluate the efficacy and safety of a multipeptide vaccine with TLR agonists and IFA.7,8
PD-1 Blockers
Talimogene laherparepvec (T-VEC) is an oncolytic immunotherapy (OI) designed to selectively replicate in tumors and produce granulocytemacrophage colony-stimulating factor (GM-CSF) to increase systemic antitumor immune responses. It is the first OI to demonstrate therapeutic benefit against melanoma, and represents a novel treatment option for melanoma with regional or distant metastases. In the phase III, randomized trial (OPTiM), the efficacy of T-VEC was evaluated in 436 patients with unresected stage 3B, 3C, or 4 melanoma, compared with GM-CSF. Data revealed that the primary endpoint of durable response rate (DRR) was met, demonstrating a significant difference in the T-VEC arm compared with the GM-CSF arm (16% vs 2%). Most frequent AEs included chills, fatigue, and pyrexia. Serious AEs occurred in 26% of patients in the T-VEC arm, and 13% in the GM-CSF arm.9PD-1 is an inhibitory T-cell co-receptor that may result in suppression of antitumor immunity. Various antibodies are being developed to inhibit the PD-1 pathway (Figure).
Lambrolizumab is a humanized, monoclonal IgG4 antibody against PD-1. In an ongoing phase Ib study of 135 patients with advanced melanoma, with or without previous ipilimumab treatment, preliminary data showed that even the lowest dose of lambrolizumab administered intravenously resulted in a high rate of sustained tumor regression. In addition to its significant antitumor activity, lambrolizumab was well-tolerated with manageable AEs.10
Combination Therapy
CTLA-4 Blockade and GM-Secreting Tumor Vaccine
CTLA-4 Blockade and PD-1 Blockade
Nivolumab is another humanized, monoclonal IgG4 antibody against PD-1. In a phase I trial of 107 patients with melanoma, data showed that nivolumab produced durable OS and responses with an acceptable safety profile. Cohorts of patients received 0.1, 0.3, 1.3, and 10 mg/kg. Median OS across all dosages was 16.8 months, and 20.3 months at the 3-mg/kg dose that was selected for phase III trials; 44% and 40% of patients remained alive at 2 and 3 years respectively; and of 29 responders who had been treated for at least one year, 16 demonstrated responses lasting one year or more. Drug-related AEs occurred in 82% of patients, and included lymphopenia, fatigue, and elevated serum lipase levels. Grade 3/4 AEs occurred in 21% of patients, and included diarrhea, endocrine disorders, and hepatitis.11Clinical and preclinical studies have begun to demonstrate evidence to support the use of combination therapies.These combinations have shown therapeutic synergy in preclinical studies. GM increases dendritic cell activation, enhances antitumor T and B cell responses, and may activate regulatory immune responses. It has shown benefit in various types of carcinoma, and is also being evaluated in phase III adjuvant trials for melanoma. In a randomized phase II trial involving 245 patients, ipilimumab plus GM significantly increased OS compared with ipilimumab alone (67.9% vs 51.2%), as well as improved OS (17.5 months vs 12.7 months), with no significant differences in toxicity. This combination of GM-CSF with ipilimumab therefore may hold promise for improving survival of patients with advanced melanoma.12This combination of drugs also appears to offer potential benefit for treatment of melanoma, compared with monotherapy. Combination immunotherapy with ipilimumab and nivolumab has also been demonstrated to produce durable tumor regression with a manageable safety profile. In a phase I trial involving 53 patients, intravenous doses of nivolumab and ipilimumab were administered every 3 weeks for 4 doses, followed by nivolumab alone every 3 weeks for 4 doses; the combined treatment was then administered every 12 weeks for up to 8 doses. In a sequenced regimen, patients previously treated with ipilimumab were treated with nivolumab every 2 weeks for up to 48 doses. Clinical activity was observed in 65% of patients, and at the maximum doses that were associated with an acceptable level of AEs, 53% of patients had an objective response, with tumor reduction of 80% or more. Drug-related grade 3/4 AEs occurred in 53% of patients in the concurrent-regimen group, but were typically reversible, and in 18% in the sequenced-regimen group. The objective response rate was increased in the concurrent-regimen group compared to the sequenced-regimen group (40% vs 20%).13
References
- Pretto F, Neri D. Pharmacotherapy of metastatic melanoma: emerging trends and opportunities for a cure.Pharmacol Ther. May 2, 2013 [Epub ahead of print].
- ClinicalTrials.gov. MEK inhibitor AZD6244 in treating patients with stage III or IV melanoma. Available at: http://clinicaltrials. gov/ct2/show/study/NCT00866177. Accessed June 16, 2013.
- O’Day S, Gonzalez R, Kim K, et al. A phase II study of the multitargeted kinase inhibitor lenvatinib in patients with advanced BRAF wild-type melanoma.J Clin Oncol. 2013;31(suppl; abstract 9026).
- Celgene. ABRAXANE meets primary endpoint of progression-free survival in phase III chemotherapy-naïve metastatic melanoma study. Available at: http://ir.celgene. com/phoenix.zhtml?c=111960&p=irolnewsArticle& ID=1740496&highlight=. Accessed June 16, 2013.
- Kharkevitch DD, Chu A, Strause LR, et al. Association of response and survival in Allovectin melanoma trials.J Clin Oncol. 2011;29(suppl; abstr 8672).
- ClinicalTrials.gov. A phase 3 pivotal trial comparing Allovectin-7 alone vs chemotherapy alone in patients with stage 3 or stage 4 melanoma. Available at: http://clinicaltrials. gov/show/NCT00395070. Accessed June 16, 2013.
- Slingluff CL, Petroni GR, Chianese-Bullock KA, et al. A multipeptide vaccine plus toll-like receptor agonists in melanoma patients, with evaluation of the vaccine site microenvironment and sentinel immunized node (Mel58; NCT01585350).J Clin Oncol. 2013;31(suppl; abstract CRA9006).
- ClinicalTrials.gov. A multipeptide vaccine plus toll-like receptor agonists in melanoma patients. Available at: http://www.clinicaltrials. gov/ct2/show/NCT01585350?term=NCT0 1585350&rank=1. Accessed June 16, 2013.
- Andtbacka RHI, Collichio FA, Amatruda T, et al. OPTiM: A randomized phase III trial of talimogene laherparepvec (T-VEC) versus subcutaneous (SC) granulocyte-macrophage colony-stimulating factor (GM-CSF) for the treatment (tx) of unresected stage IIIB/C and IV melanoma.J Clin Oncol. 2013;31(suppl; abstract LBA9008).
- Ribas A, Robert C, Daud A, et al. Clinical efficacy and safety of lambrolizumab (MK- 3475, Anti-PD-1 monoclonal antibody) in patients with advanced melanoma.J Clin Oncol. 2013;31(suppl; abstract 9009).
- Sznol M, Kluger HM, Hodi S, et al. Survival and long-term follow-up of safety and response in patients (pts) with advanced melanoma (MEL) in a phase I trial of nivolumab (anti-PD-1; BMS-936558; ONO-4538).J Clin Oncol. 2013;31(suppl; abstract TPS3125).
- Hodi FS, Lee SJ, McDermott DF, et al. Multicenter, randomized phase II trial of GMCSF (GM) plus ipilimumab (Ipi) versus Ipi alone in metastatic melanoma.J Clin Oncol. 2013;31(suppl; abstract CRA9007).
- Wolchok JD, Kluger H, Callahan MK, et al. Nivolumab plus ipilimumab in advanced melanoma.N Engl J Med. 2013;Jun 2 [Epub ahead of print].