FDA Grants Priority Review to Epcoritamab for R/R Follicular Lymphoma
If FDA-approved, epcoritamab would be the first and only subcutaneous bispecific antibody indicated for the treatment of adult patients with relapsed/refractory follicular lymphoma after 2 rounds of previous therapy.
- The FDA has prioritized the review of the supplemental biologics license application (sBLA) for epcoritamab-bysp (Epkinly) for treating adult relapsed or refractory (R/R) follicular lymphoma (FL) after at least 2 lines of therapy.
- This designation accelerates the review process, shortening it to 6 months compared to the standard 10-month review period.
- Findings from the phase 1/2 EPCORE NHL-1 trial (NCT03625037) support the regulatory decision, indicating that subcutaneous epcoritamab led to deep and durable responses in patients with R/R FL.

The FDA has granted priority review of the sBLA for epcoritamab for the treatment of adult R/R FL after at least 2 lines of therapy.1
Findings from the phase 1/2 EPCORE NHL-1 trial support this regulatory decision as subcutaneous epcoritamab led to deep and durable responses and demonstrated high overall and complete responses (CR) among patients with R/R FL. Results from a cohort of 128 adult patients revealed that at a median follow-up of 17.4 months, the study's primary end point of overall response rate (ORR) was 82% with a CR rate of 63%. The median time to response and CR were 1.4 months and 1.5 months, respectively.2
Among prespecified high-risk subgroups, including patients refractory to prior treatments, the ORR and CR rates remained generally consistent with the overall study population. Importantly, the median duration of response and duration of CR were not yet reached, and an estimated 85% and 74% of patients who achieved a CR remained responsive to treatment at 12 and 18 months, respectively.
“Despite new treatment options, follicular lymphoma remains incurable and difficult to treat. Unfortunately, relapse is common and additional lines of treatment are needed," said Mariana Cota Stirner, MD, PhD, vice president, therapeutic area head for hematology, AbbVie, in a press release.1 "Together with our partner Genmab, we are committed to further advancing epcoritamab as a core lymphoma therapy."
No new safety signals emerged in this cohort, providing reassurance regarding the agent’s tolerability. The most common treatment-emergent adverse event (TEAE) was cytokine release syndrome (CRS), which was observed in 67% of patients at varying grades of severity. Notably, no cases of immune effector cell-associated neurotoxicity syndrome were reported.2
Moreover, common TEAEs, including injection-site reactions, COVID-19, fatigue, neutropenia, diarrhea, and pyrexia, were manageable. However, TEAEs leading to treatment discontinuation were observed in 19% of patients and death related to TEAEs occurred in 10% of patients.
Epcoritamab is a T-cell engaging bispecific antibody given to patients subcutaneously. The agent was previously granted an FDA breakthrough therapy designation in November 2023. At the same time, the breakthrough therapy designation was submitted to the European Medicines Agency (EMA) in November 2023.1
With this priority review, the review period for epcoritamab has been shortened to 6 months compared with 10 months for standard review.
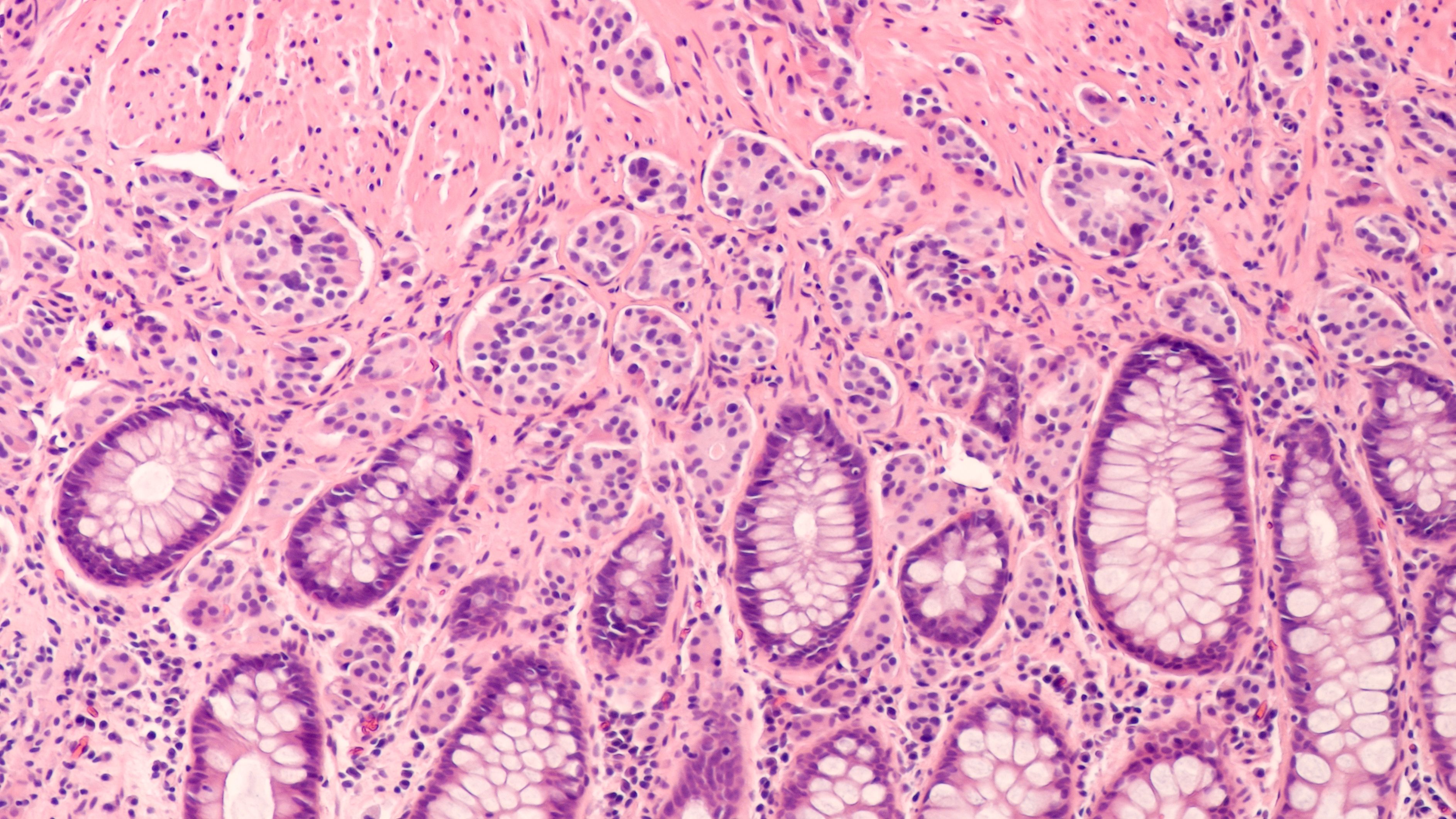
Lymphomas: © David A Litman - stock.adobe.com
If granted FDA approval, epcoritamab would become the first and only subcutaneous bispecific antibody for the treatment of adult patients with R/R FL after 2 rounds of previous therapy. This would mark its second indication following FDA and EMA approval for treating R/R third-line diffuse large B-cell lymphoma.
Background of EPCORE NHL-1
The EPCORE NHL-1 trial is an open-label, multicenter study evaluating the safety and preliminary efficacy of subcutaneous epcoritamab when used for the treatment of patients with relapsed, progressive, or refractory CD20-positive mature B-cell non-Hodgkin lymphoma, including FL, after 2 or more lines of systemic therapy.3 The study consists of 3 parts, including dose escalation, dose expansion, and dose optimization.
Enrollment was open to patients with acceptable renal and liver functions and an ECOG performance status of 0 to 2. Patients were eligible for enrollment in the trial if they had no signs of primary central nervous system (CNS) lymphoma or CNS involvement, a known past or current malignancy other than inclusion diagnosis, clinically significant cardiovascular disease, a history of autoimmune disease or immunosuppression, or active hepatitis B, hepatitis C, or HIV infection.
The expansion part of the study enrolled additional patients to further explore the safety and efficacy of epcoritamab in 3 cohorts which each included patients with different types of R/R B-cell non-Hodgkin lymphoma. In the optimization part, investigators are assessing the potential for alternative step-up dosing regimens to help further minimize grade 2 CRS and prevent grade ≥3 CRS.
The expansion portion had the primary end point of ORR and secondary end points of duration of response, CR rate, duration of CR, progression-free survival, time to response as determined by the Lugano criteria, overall survival, time to next therapy, and rate of minimal residual disease negativity. For the optimization part of the study, the primary end point was the rate of ≥ grade 2 CRS events and all grade CRS events from the first epcoritamab dose through 7 days after patients received the second full dose of epcoritamab.
REFERENCES:
U.S. Food and Drug Administration (FDA) grants priority review of epcoritamab (EPKINLY®) for difficult-to-treat relapsed or refractory follicular lymphoma (FL). News release. AbbVie. February 27, 2024. Accessed February 27, 2024. http://tinyurl.com/ymebu8ku
New data for bispecific antibody epcoritamab (DuoBody® CD3xCD20) shows strong, durable treatment response for patients with difficult-to-treat relapsed/refractory (R/R) follicular lymphoma (FL). News release. AbbVie. December 9, 2023. Accessed February 27, 2024. http://tinyurl.com/mr3ucswa
First-in-human (FIH) trial in patients with relapsed, progressive or refractory B-cell lymphoma (EPCORE NHL-1). ClinicalTrials.gov. Updated February 16, 2024. Accessed February 27, 2024. https://www.clinicaltrials.gov/study/NCT03625037
Does Odronextamab Show Hope in FL and DLBCL Despite Regulatory Hurdles?
November 5th 2024Despite regulatory challenges from the FDA, odronextamab has received European approval for the treatment of patients with relapsed/refractory follicular lymphoma or diffuse large B-cell lymphoma following 2 prior treatments.
Read More
Phase 3 Trial of Tafasitamab in Follicular Lymphoma Meets Primary End Point
August 16th 2024The phase 3 inMIND trial evaluating tafasitamab in combination with lenalidomide and rituximab in relapsed or refractory follicular lymphoma showed promising progression-free survival findings, according to topline results.
Read More