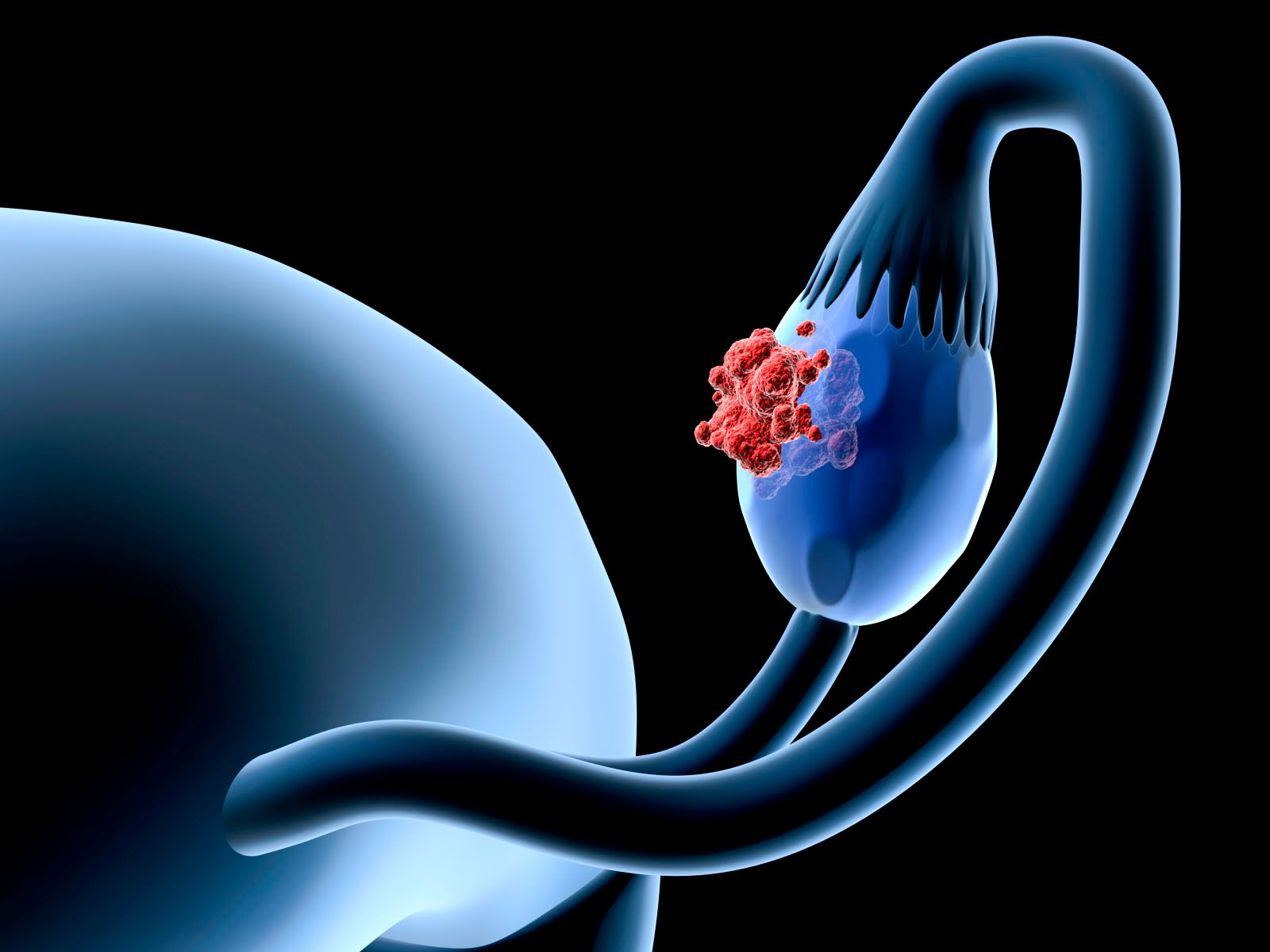
Early Research Under Way to Improve Drug Delivery in Ovarian Cancer
Targeted agents have become available in recent years to treat many major cancers, but for women with ovarian cancer, standard treatment following cytoreductive surgery remains systemic intravenous/intraperitoneal chemotherapy with a platinum agent and a taxane. Approximately 80% of women who receive first-line treatment with this platinum-based regimen experience relapsed disease. However, early research indicates that more and better options may be on the way.
Ovarian Cancer
Targeted agents have become available in recent years to treat many major cancers, but for women with ovarian cancer, standard treatment following cytoreductive surgery remains systemic intravenous/intraperitoneal chemotherapy with a platinum agent and a taxane.1Approximately 80% of women who receive first-line treatment with this platinum-based regimen experience relapsed disease. However, early research indicates that more and better options may be on the way.2
Treatment for women with platinum-sensitive epithelial ovarian cancer is often another platinum-based regimen. Women with ovarian cancer that is considered platinum-refractory or platinum-resistant (disease progression while taking the drug or recurrence within 6 months of completing a platinum-containing regimen) are typically treated with one of a long-list of non-platinum agents, all of which have fairly low response rates.2The possible exception is nab-paclitaxel, which National Comprehensive Cancer Network guidelines1 say has an overall response rate of 64%.
In November 2014, the FDA approved bevacizumab (Avastin) combined with a chemotherapy agent for women with platinum-resistant, recurrent ovarian cancer. Bevacizumab plus chemotherapy may also be an option for women with platinum-sensitive recurrence.1Bevacizumab selectively targets the vascular endothelial growth factor receptor to inhibit angiogenesis.
Another angiogenesis agent currently in an early clinical trial3for ovarian cancer uses recombinant thrombospondin-1 type I repeats (3TSR). Binding of 3TSR to the CD36 receptor inhibits the tumor’s ability to form new blood cells. Russell and colleagues used 3TSR to treat mice with ovarian cancer tumors prior to chemotherapy. They observed tumor shrinkage and destruction of abnormal blood vessels. The result was enhanced blood flow to the ovarian tumor, which increased uptake of chemotherapy and allowed the use of smaller doses.
Ways of improving chemotherapy delivery are also being investigated. A study published in September 2014, showed that more aggressive ovarian malignancies expressed higher levels of gelsolin, a protein that appears to protect cancer cells against cisplatin. Yet when the investigators inserted fragments of gelsolin into the chemo-resistant cancer cells, they became sensitized to cisplatin.4In a press release, study collaborator Dar-Bin Shieh, MD, National Cheng Kung University, Taiwan, hailed the discovery as “a promising avenue for developing a new therapy to reduce chemo-resistance in women with this deadly disease.”5
Growing attention is also being given to folate receptors (FRs), which are overexpressed on the cell surface in almost all epithelial ovarian cancers but have relatively low expression in normal tissues.6Folate is essential for cell division and is transported by the reduced folate carrier (RFC) or the FR pathway. Several clinical trials have evaluated farletuzumab (MORAb-003), an anti-FR antibody highly selective for FRα. In a phase III study, farletuzumab was combined with carboplatin and a taxane and compared with placebo in 1100 women with relapsed platinum-sensitive epithelial ovarian cancer. The study found no significant differences between the arms. Another phase III study evaluated farletuzumab with paclitaxel in women with platinum-resistant ovarian cancer, but the study was prematurely discontinued due to lack of efficacy. Researchers are stratifying data by FR receptor status to determine whether or not the drug may be more effective in women with high FRα expression.6
Vintafolide (EC145) consists of a folate conjugate highly selective for FR coupled with a vinca alkaloid. In the PRECEDENT trial, a combination of vintafolide and pegylated liposomal doxorubicin (PLD) in women with platinum-resistant ovarian cancer improved median progression-free survival by 2.3 months, which was significant. The greatest benefit in progression-free survival was observed in women whose tumors were all FR positive, who had a 4-month improvement.6However, the phase III PROCEED study was suspended after interim data showed it was unlikely to meet its primary endpoint, and it is not clear whether or not the manufacturers will pursue any further study of vintafolide in ovarian cancer.7
One group has been evaluating whether or not intraperitoneal injections of poly(ethylene glycol)-block-poly(ε-caprolactone)(PEG-b-PCL) micelles containing chemotherapy agents could allow for regional and sustained drug release in ovarian cancer.8Thus far, the only studies conducted have been in vitro and in mouse models. However, micelles delivering a 3-drug combination of paclitaxel, cyclopamine, and gossypol reduced the volume of ovarian tumors in mice significantly more than paclitaxel alone. Mice treated with the 3-drug micelles also had improved survival.8
Preclinical findings will need to be confirmed in clinical trials to determine the efficacy and safety of these agents. The premature discontinuation of phase III trials of FR inhibitors suggests that the use of this class may be tentative. Determining which of these treatments will make it into the clinical setting remains many years away.
References
- National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: ovarian cancer including fallopian tube cancer and primary peritoneal cancer. v 3.2014. http://www.nccn.org/professionals/physician_gls/pdf/ovarian.pdf. Updated May 9, 2014. Accessed February 8, 2015.
- National Cancer Institute. Ovarian epithelial, fallopian tube, and primary peritoneal cancer treatment (PDQ): recurrent or persistent ovarian epithelial, fallopian tube, and primary peritoneal cancer treatment. http://www.cancer.gov/cancertopics/pdq/treatment/ovarianepithelial/HealthProfessional/page6. Updated December 23, 2014. Accessed February 8, 2015.
- Russel S, Duquette M, Liu J, et al. Combined therapy with thrombospondin-1 type I repeats (3TSR) and chemotherapy induces regression and significantly improves survival in a preclinical model of advanced stage epithelial ovarian cancer.FASEB J.2015;29:576-588.
- Abedini MR, Wang PW, Haung YF, et al. Cell fate regulation by gelsolin in human gynecologic cancers.Proc Natl Acad Sci U S A.2014;111:14442-14447.
- Ottawa Hospital Research Institute. A way to kill chemo-resistant ovarian cancer cells: cut down its protector [press release]. http://www.ohri.ca/newsroom/newsstory.asp?ID=531. Published September 24, 2014. Accessed February 8, 2015.
- Marchetti C, Palaia I, Giorgini M, et al. Targeted drug delivery via folate receptors in recurrent ovarian cancer: a review.Onco Targets Ther.2014;7:1223-1236.
- Merck. Merck and Endocyte announce withdrawal of conditional marketing authorization applications for vintafolide and companion imaging components, etarfolatide and intravenous (IV) folic acid in Europe [press release]. http://www.mercknewsroom.com/news-release/oncology-newsroom/merck-and-endocyte-announce-withdrawal-conditional-marketing-authoriz. Published May 19, 2014. Accessed February 9, 2015.
- Cho H, Lai TC, Kwon GS, et al. Poly(ethylene glycol)-block-poly(ε-caprolactone) micelles for combination drug delivery: evaluation of paclitaxel, cyclopamine and gossypol in intraperitoneal xenograft models of ovarian cancer.J Control Release.2014;166:1-9.