Atezolizumab Increases PFS in Front-Line FOLFIXIR Plus Bevacizumab Treatment in Patients with mCRC
Adding atezolizumab to first-line FOLFOXIRI with bevacizumab is shown to be a safe treatment option and improves progression-free survival in patients with metastatic colorectal cancer.
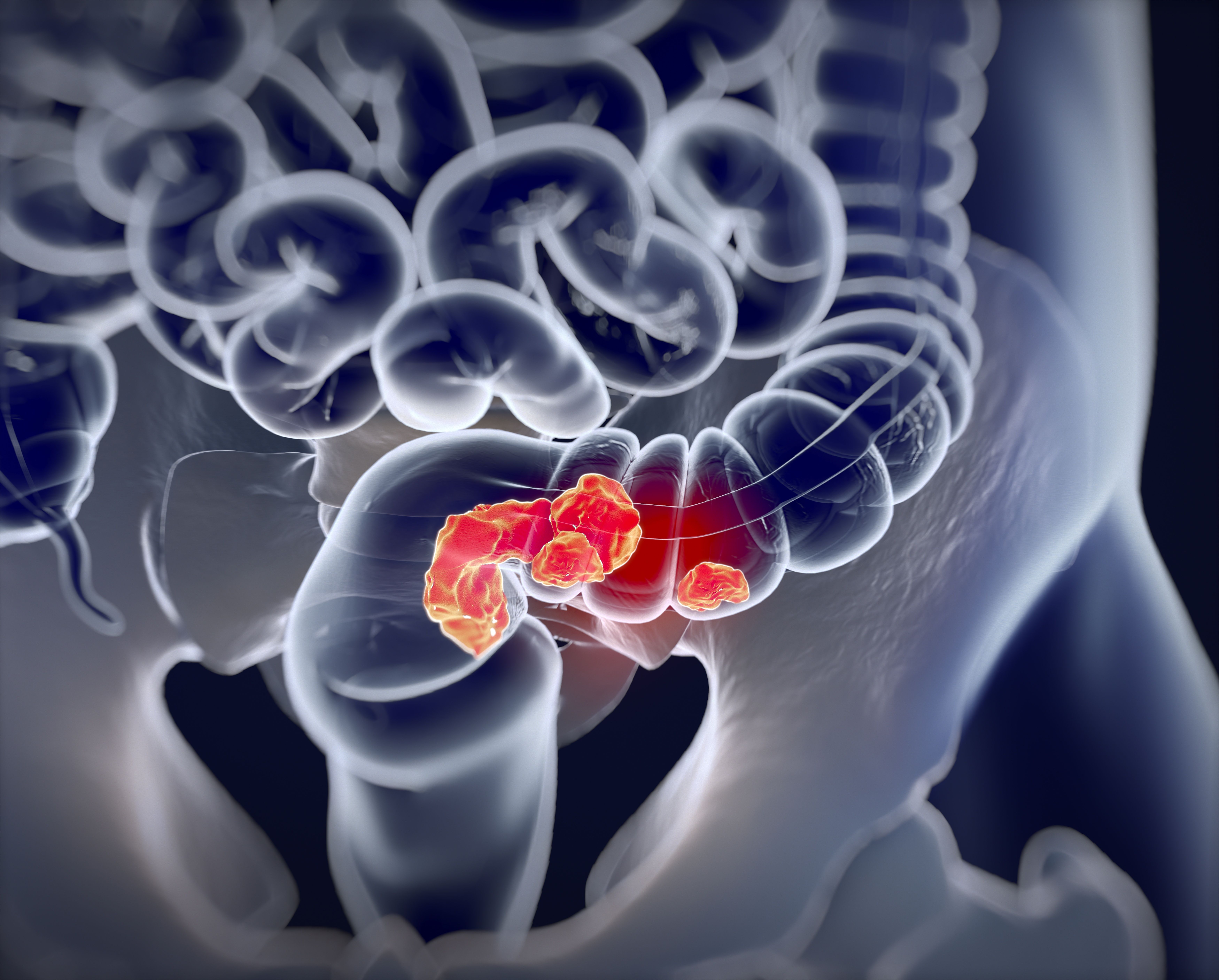
Patients with metastatic colorectal cancer demonstrated an improved progression-free survival (PFS) and had a tolerable safety profile with the addition of atezolizumab (Tecentriq) to first-line FOLFOXIRI (fluorouracil, leucovorin, oxaliplatin, and irinotecan) plus bevacizumab (Avastin).1
At the data cutoff of August 1, 2021, the median PFS was 13.1 months (80% CI, 12.5-13.8) for patients in the atezolizumab group vs 11.5 months (80% CI, 10.0-12.6) for patients in the control group (hazard ratio [HR], 0.69; 80% CI, 0.56-0.85; P = .012; adjusted HR, 0.70; 80% CI, 0.57-0.87; log-rank test P = .018). Patients had a median follow-up of 19.9 months (range, 17.3-23.9).
Patients with metastatic colorectal cancer who have proficient mismatch repair (pMMR) or microsatellite stable (MSS) have not seen much clinical benefit when treated with immune checkpoint inhibitors in previous studies. However, the combination of FOLFOXIRI and bevacizumab seem to have increased the immunogenicity of pMMR or MSS tumors. Investigators believed to see additional benefit when deciding to add the anti-PD-L1 agent, atezolizumab, to first-line FOLFOXIRI plus bevacizumab in this patient population.
Investigators in the multicenter, open-label, randomized, controlled phase 2 AtezoTRIBE study (NCT03721653) randomly assigned 218 patients 2:1 to receive atezolizumab plus FOLFOXIRI plus bevacizumab (n = 145) or to the control group (n = 73) between November 30, 2018, and February 26, 2020. The experimental group received received intravenous (IV) atezolizumab at 840 mg dose plus first-line IV FOLFOXIRI plus 5 mg/kg IV bevacizumab, and the control group received the same regimen without the addition of atezolizumab. Patients received combination treatments for up to eight 14-day cycles followed by maintenance with FOLFOXIRI with or without atezolizumab. Patients were treated until disease progression, unacceptable adverse events (AEs), or withdrawal.
The study enrolled patients between the age of 18 and 70 years with an ECOG performance score of 0 to 2 and patients between the age of 71 and 75 years with an ECOG performance score of 0. Patients were required to have histologically confirmed, unresectable preciously untreated metastatic colorectal cancer and have adequate organ function. Patients were recruited from 22 centers throughout Italy. Patients were stratified by which center they were recruited from, ECOG performance status, their primary tumor site, and by any previous adjuvant therapy they may have received.
The primary end point of the study was PFS, analyzed by the intention-to-treat principle. Safety was observed and recorded in patients who received at least one dose of the study treatment.
The most frequent grade 3 or 4 AEs were neutropenia, reported in 59 (42%) of 142 patients in the atezolizumab group vs 26 (36%) of 72 patients in the control group; diarrhea in 21 patients (15%) vs 9 patients (13%), respectively; and febrile neutropenia in 14 patients (10%) vs 7 patients (10%), respectively. Investigators observed serious AEs in in 39 (27%) patients in the atezolizumab group and in 19 (26%) patients in the control group.
There were 2 (1%) treatment-related deaths reported in the atezolizumab group and 0 treatment related deaths in the control group. The 2 deaths in the experimental group were caused by an acute myocardial infarction and a bronchopulmonary hemorrhage.
Investigators concluded that adding atezolizumab to first-line FOLFOXIRI with bevacizumab is a safe treatment option and improves PFS in patients with metastatic colorectal cancer.
References
Antoniotti C, Rossini D, Pietrantonio F, et al. Upfront FOLFOXIRI plus bevacizumab with or without atezolizumab in the treatment of patients with metastatic colorectal cancer (AtezoTRIBE): a multicentre, open-label, randomised, controlled, phase 2 trial. Published online May 27, 2022. Lancet Oncol. 2022;S1470-2045(22)00274-1. doi:10.1016/S1470-2045(22)00274-1
Phase 3 Trials of Botensilimab/Balstilimab Move Forward, Despite FDA's Approval Setback
July 18th 2024Agenus was advised by the FDA against filing for accelerated approval of botensilimab plus balstilimab for relapsed/refractory microsatellite stable metastatic colorectal cancer without liver metastases.
Read More