Analysis Supports Consolidative Stem Cell Transplant for CD30+ PTCL Post A+CHP
Though the benefit of consolidative stem cell transplant for patients who received A+CHP appeared less pronounced vs those treated with the CHOP regimen, the method is still supported for patients with CD30-positive peripheral T-cell lymphomas.
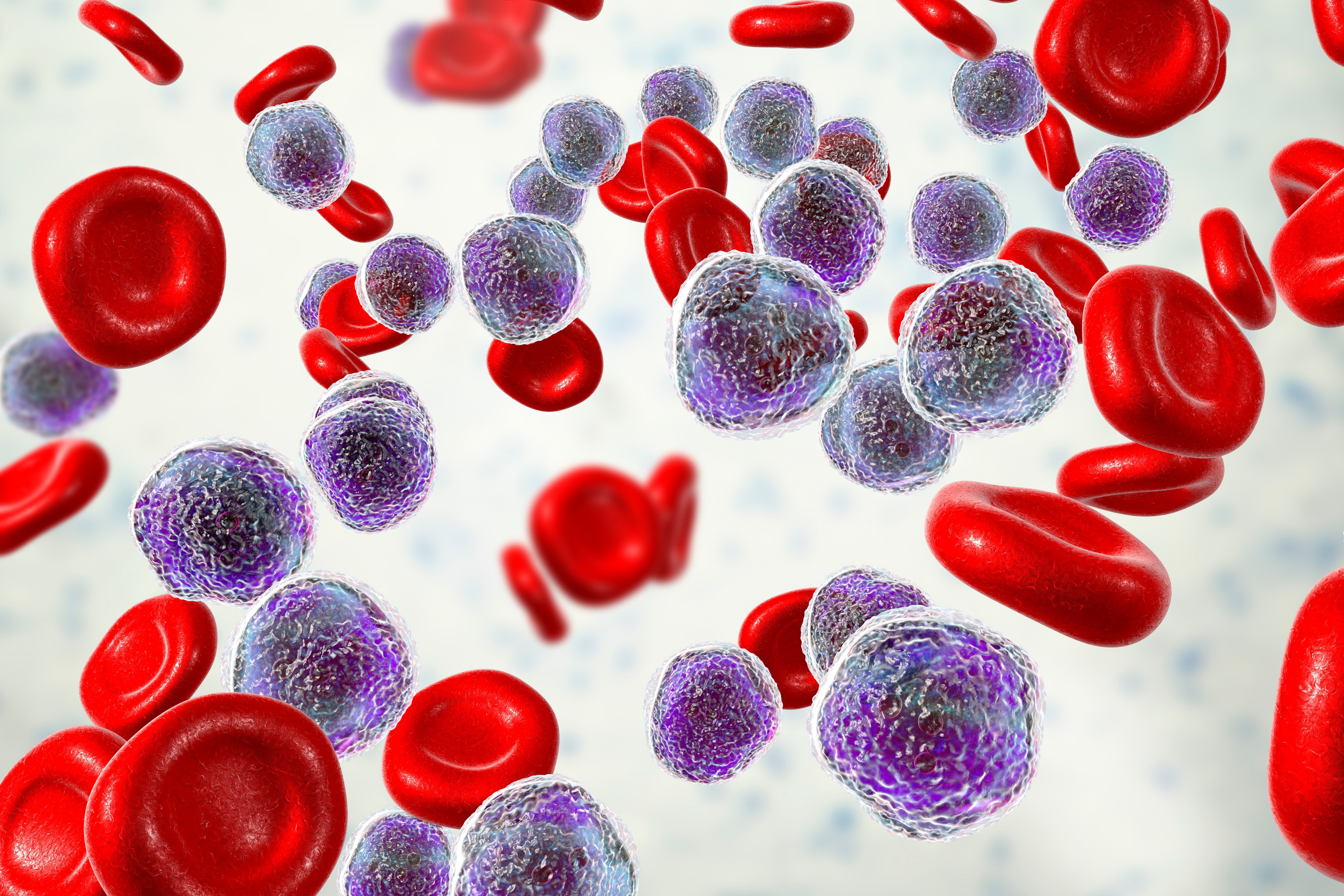
Image Credit: © Dr_Microbe stock.adobe.com
Data from an exploratory subgroups analysis support the use of consolidative stem cell transplant (SCT) in patients with CD30-positive peripheral T-cell lymphomas (PTCL) who achieve complete response (CR) after receiving treatment with brentuximab vedotin (Adcetris) plus cyclophosphamide, doxorubicin, and prednisone (A+CHP).1
Previously, findings from the double-blind, randomized, phase 3 ECHELON-2 study (NCT01777152) showed improvements in progression-free survival (PFS), overall survival, CR, and overall response rate when patients with PTCLs were treated with frontline A+CHP.2 As a sustained benefit at 5 years of follow-up was demonstrated, the FDA has granted approval to brentuximab vedotin in this indication, as well as in other jurisdictions.
However, there have been recent improvements for frontline therapies, causing experts to reevaluate the role of consolidative SCT.1 To further examine the impact of consolidative SCT on PFS in patients with previously untreated CD30-positive PTCL, experts conducted an exploratory subgroups analysis. In the analysis, patients were in CR after frontline treatment with A+CHP or cyclophosphamide, doxorubicin, vincristine, and prednisone.
The exploratory analyses enrolled adult patients with previously untreated CD30+-positive PTCL, (anaplastic large cell lymphoma [ALCL] or non-ALCL), except for ALK-positive systemic ALCL. Patients were randomized to receive either A+CHP or cyclophosphamide, doxorubicin, prednisone, and vincristine (CHOP) for 6 or 8 cycles. Patients were able to have consolidative SCT or radiotherapy, as permitted by the investigator, after treatment with their intent specified prior to the first cycle of treatment.
The primary end point in the study was PFS. Additionally, patients who discontinued treatment due to adverse events (AEs) were included in the analyses if they were in a CR at the end of treatment.
For patients with ALK-positive sALCL or non-ALCL who received A+CHP, 114 patients of 177 (64%) were in a CR at the end of therapy. This included 67% of patients (76/113) with ALK-positive sALCL and 59% (38/64) with non-sALCL. A total of 27 of 76 of patients (36%) with ALK-positive sALCL and 11 of 38 (29%) patients with non-ALCL underwent consolidative SCT.
Among those who underwent SCT, the median age was lower vs patients who did not undergo SCT, regardless of subtype. For patients with ALK-positive sALCL, the median age was 50 years vs 59 years and for patients with non-sALCL ages were 57 years vs 66 years. Further, there was no difference in AE profile for patients who underwent SCT vs those who did not undergo SCT.
The results of the study showed that the median PFS follow-up was 47.57 months with a hazard ratio of 0.36 (95% CI, 0.17-0.77), equating to a 64% reduction in the risk of a PFS event in all patients who underwent SCT. At 3 years, the estimated PFS for patients who underwent SCT was 80.4% vs 54.9% in patients who did not undergo SCT. Then at 5 years, the estimated PFS was 65.3% vs 46.4%, respectively.
In patients who underwent SCT, the median PFS was not reached vs 55.66 months in patients who did not undergo SCT. The use of SCT in both ALK-positive ALCL and non-ALCL subgroups was favored, according to the PFS data.
This analysis supports the benefit of consolidative SCT for patients who received A+CHP. However, study authors in Blood Adv note that the benefit appeared less pronounced among patients treated with the CHOP regimen.
According to the study authors, this exploratory analysis shows that even with superior frontline therapies for patients with CD30-positive PTCL using A+CHP, consolidative SCT should still be considered. Further studies are needed to provide additional context for SCT in this patient population.
REFERENCES:
Savage KJ, Horwitz SM, Advani R, et al. Role of stem cell transplant in CD30+ PTCL following frontline brentuximab vedotin plus CHP or CHOP in ECHELON-2. Blood Adv. 2022;6(19):5550-5555. doi:10.1182/bloodadvances.2020003971
ECHELON-2: A comparison of brentuximab vedotin and CHP with standard-of-care CHOP in the treatment of patients with CD30-positive mature T-cell lymphomas (ECHELON-2). ClinicalTrials.gov. Updated November 30, 2021. Accessed July 19, 2023. https://clinicaltrials.gov/study/NCT01777152