Addition of 177Lu-PSMA-617 to Enzalutamide Improves PSA-PFS in mCRPC
Adding 177Lu-PSMA-617 to enzalutamide improved prostate-specific antigen progression-free survival in patients with metastatic castration-resistant prostate cancer.
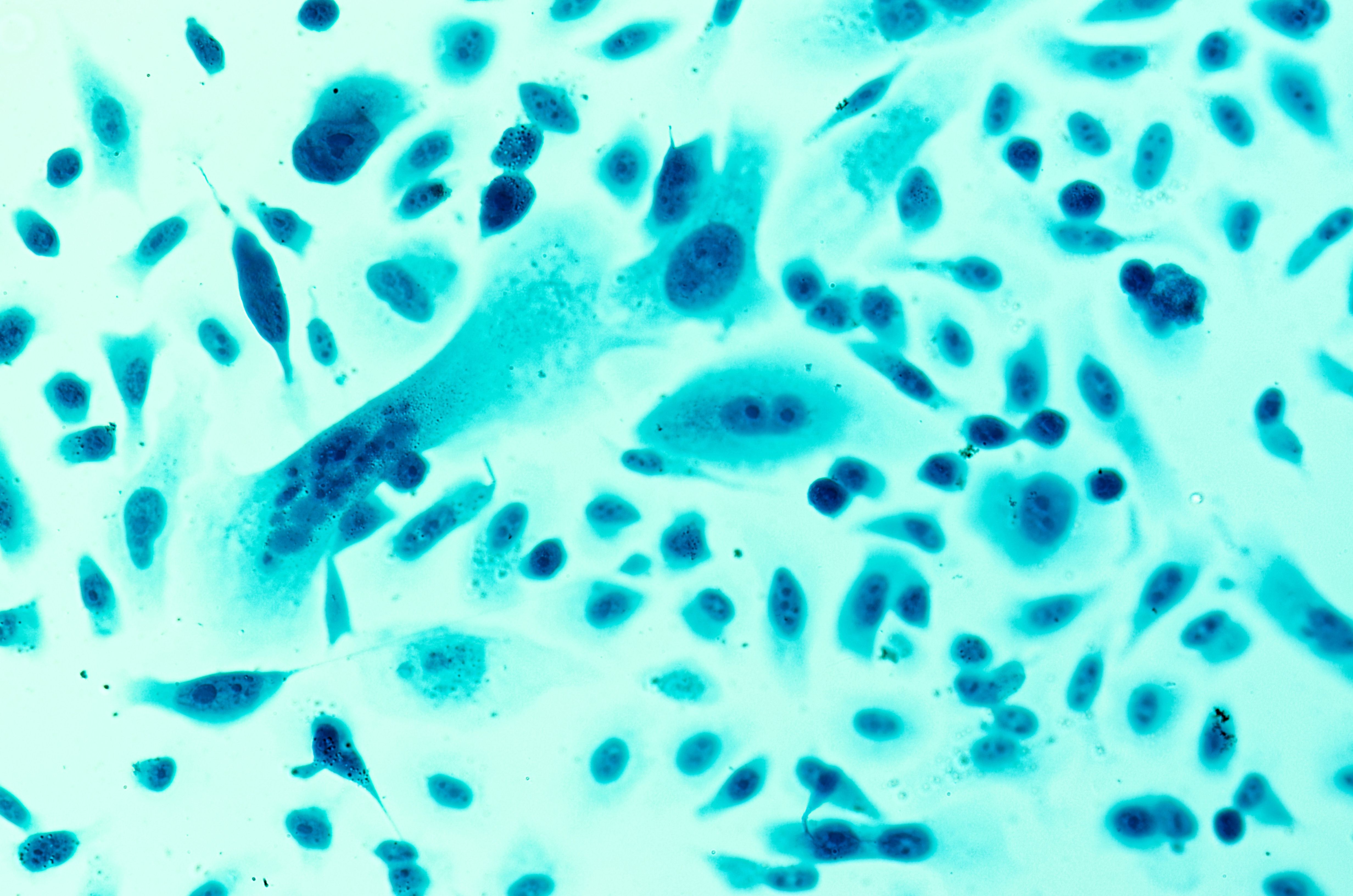
prostate cancer under the microscope: © heitipaves - stock.adobe.com
Interim results from the phase 2 ENZA-p study (NCT04419402) show that adding 177Lu-PSMA-617 (Pluvicto) to enzalutamide (Xtandi) significantly enhances prostate-specific antigen progression-free survival (PSA-PFS) in patients with metastatic castration-resistant prostate cancer (mCRPC), according to findings presented at the European Society of Medical Oncology (ESMO) Congress, Madrid, Spain.1
“This is the first randomized trial combining an androgen receptor signaling inhibitor, enzalutamide, with 177Lu-PSMA-617. It provides strong evidence for an enhanced anti-cancer effect with the combination of enzalutamide and 177Lu-PSMA-617 based on the primary end point, PSA-PFS,” said Louise Emmett, MD, FRACP, during an oral presentation of the findings at the ESMO meeting. Emmett is the director of theranostics and nuclear medicine at St. Vincent’s Hospital in Sydney, Australia.
Data from the study showed a median PSA-PFS of 13 months with the combination therapy compared with 7.8 months with enzalutamide alone (HR, 0.43; 95% CI, 0.29-0.63; P = .00001). Median radiographic PFS was 16 months with the combination therapy compared with 12 months for enzalutamide alone (HR, 0.67; 95% CI, 0.44-1.01).1
Further, PSA 50% (decrease ≥50% from baseline) response rates were 93% (77/83) in the combination arm, compared with 68% (54/79) for enzalutamide alone (P < .001). PSA 90% (decrease ≥90% from baseline) response rates were 78% (65/83) among those in the combination arm compared with 37% (29/79) among those who received enzalutamide alone (P < .001).1
In total, the ENZA-p study included 162 patients with mCRPC. Patients were randomly assigned 1:1 to 160 mg of enzalutamide alone (n = 79) or 160 mg enzalutamide plus 7.5 GBq 177Lu-PSMA-617 (n = 83) delivered in 2 or 4 doses. Those included in the combination therapy arm underwent 2 doses with 177Lu-PSMA-617 with SPECT with 2 additional doses for those with persistent PSMA-positive disease detected at 92-day follow-up. In total, 81% of patients in the combination arm received 4 doses of 177Lu-PSMA-617.1
Emmett commented in the presentation, “We used 2 to 4 doses of Lu-PSMA in the ENZA-p trial, but 2 to 6 doses may further improve progression-free survival, particularly in those patients who have a high proportion of androgen persistent clones.”
The primary end point of the study was PSA-PFS. Secondary end points included radiological PFS, PSA50%, PSA90%, adverse events (AEs), and overall survival (OS).2 Median follow-up among all patients included in the study was 20 months.
Serious AEs were reported in 35% (28/79) of patients who received enzalutamide alone, compared with 33% (27/81) of patients who received enzalutamide with 177Lu-PSMA-617. Grade 4 or 5 AEs were reported among 4% (3/79) of patients in the enzalutamide monotherapy arm, compared with 6% (8/81) of patients in the combination arm.1
In the presentation conclusion, Emmett noted, “I think this is going to become more important as we move this radiation treatment earlier in the disease paradigm to hormone sensitive prostate cancer. It [has] the potential to reduce toxicity by only administering if persistent PSMA-avid disease is present on the PSMA-PET or SPECT images.”
Emmett also added that there is planned follow-up of PFS and OS in the study until July 2024.