Evolving Paradigms in Soft Tissue Sarcoma: Introduction
This section covers the Introduction and Epidemiology, Risk Factors, Detection and Diagnosis, and Staging and Prognosis sections of the current Evolving Paradigms in Soft Tissue Sarcoma issue.
Introduction and Epidemiology
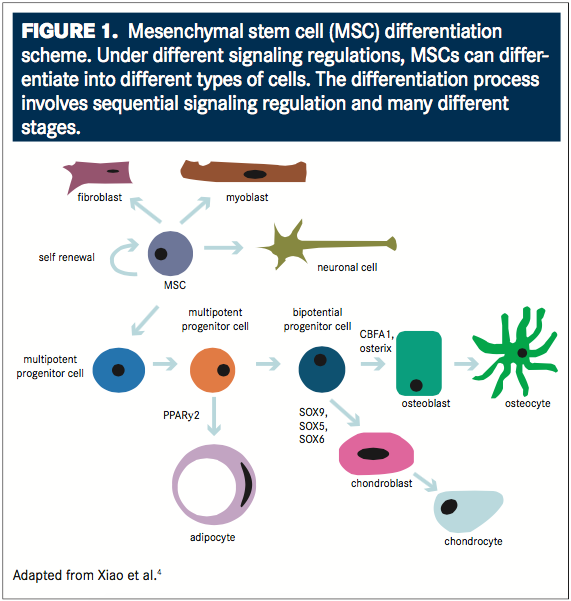
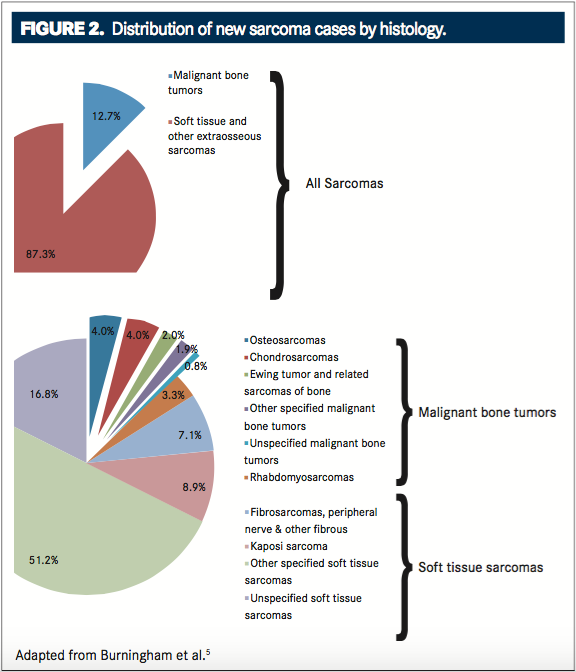
Soft tissue sarcomas (STS) are tumors arising from the mesenchymal cells (FIGURE 1) and occur in fat, joints, muscles, blood vessels, nerves, and deep skin tissue (FIGURE 2).1According to classification by the World Health Organization (WHO), there are more than 50 histologic subtypes, and although STS are more prevalent than osteosarcomas, they account for only 1% to 2% of all malignancies.1,2It was estimated that 12,310 people would be diagnosed with STS and 4990 people would die from this cancer in 2016.3New cases of STS account for only 0.7% of all new cancer cases. The heterogeneity and rarity of STS has made evidence-based treatment difficult. As the understanding of tumor biology increases, new approaches to management of STS focus on selectively treating distinct subtypes.
Risk Factors
Although the cause of most STS is unknown, known risk factors are associated with the disease.6These include genetic syndromes, radiation, and chemical exposure.5Neurofibromatosis, also known as von Recklinghausen’s disease, is an inherited syndrome that increases the cumulative lifetime risk for nerve sheath tumors to 10%. It results from the dysfunction of the NF1 gene. Li-Fraumeni syndrome and hereditary retinoblastoma are also genetic syndromes that are associated with STS and result from germline mutations of tumor suppressor genes, specifically, TP53 and RB1, respectively.5The most common subtype associated with hereditary retinoblastoma is leiomyosarcoma followed by fibrosarcomas.7In a cohort of 963 patients with hereditary retinoblastoma, Kleinerman et al found that 33% of diagnosed STS were leiomyosarcomas.7
In addition to genetic syndromes, high-dose radiotherapy increases the risk of secondary STS.5In a 2008 study, Penel et al evaluated 658 patients with STS to determine the frequency of etiologic factors.6Of the patients, 3.3% had radiation-induced STS. The time from primary cancer to secondary STS averaged 10 years.
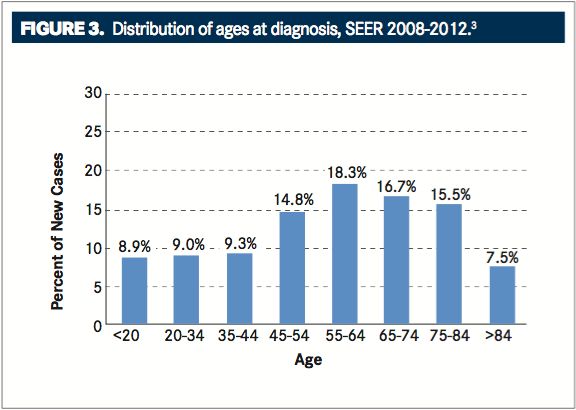
Results from studies evaluating chemical exposure in association with STS vary.8When correlations are found, they are usually associated with herbicides and chlorophenols. Sex and age are also risk factors for STS. Overall, men have a slightly higher risk for STS than women (1.23:1.00 ratio, respectively), and diagnosis occurs more frequently in patients >55 years, with the mean age at diagnosis being 59 years (FIGURE 3).4,5
Detection and Diagnosis
STS are solid tumors and present as a new or growing lump.1The lump is usually painless, and the most common site for STS are the extremities (33%), followed by the trunk (14%) and retroperitoneum (19%).1,9,10A total of 8% of STS occur in the head and neck.10When located in the abdomen, STS may obstruct and cause bleeding of the bowels or stomach.9This can present as abdominal pain and blood in stool or vomit.
When a lump is present, imaging tests assist with diagnosis and staging.8,11Although traditional x-rays can rule out bone tumors and ultrasounds can differentiate between cysts and tumors, magnetic resonance imaging (MRI) is the standard imaging modality for STS, especially STS of the extremities, pelvis, and trunk. Computed tomography (CT) can be used for imaging STS of the retroperitoneum, and chest CT is useful for determining metastasis, since a majority of STS metastasize to the lungs.10,11Abdominal STS may metastasize to the liver or peritoneum, and lymph node metastases are rare.8Positron emission tomography is also an effective imaging modality, but its cost-effectiveness is undetermined.8,11
Besides imaging tests, biopsy is also required for the diagnosis and grading of STS.8,11Core needle biopsy is the preferred method because fine needle aspiration does not always provide a sufficient amount of tissue for accurate diagnosis. In cases when the tumor is superficial and smaller than 3 cm, removal of the entire tumor during biopsy may be more practical.8
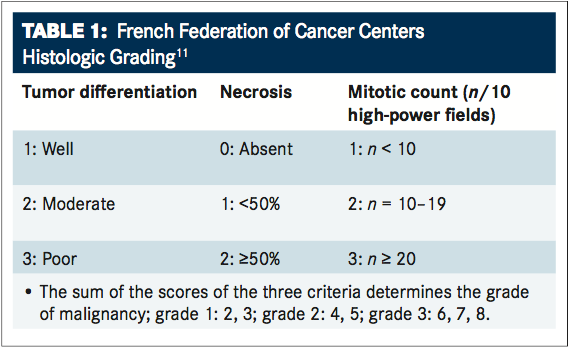
Histologic diagnosis is based on biopsy samples and is classified using the WHO classification of tumors.1,8,11Differential diagnosis includes other malignant lesions, desmoids, and benign lesions.8Biopsy samples also provide information for grading.12Two systems are used for grading STS: the French Federation of Cancer Centers (FFCC) and the National Cancer Institute (NCI). Both include 3 tumor characteristics. The NCI system includes tumor histology, location, and necrosis, and the FFCC includes tumor differentiation, mitosis count, and necrosis (TABLE 1).11In a study comparing both systems, researchers evaluated 410 patients with STS and found that the FFCC system better predicted tumor mortality and metastasis.13
Ancillary diagnostic techniques include molecular genetic testing: immunohistochemistry, cytogenetics, and reverse transcription polymerase chain reaction (RT-PCR).8Molecular genetic testing identifies genetic abnormalities associated with STS subtypes and may also assist with prognosis.12For example, the fusion of the genes PAX3-FKHR or PAX7-FKHR is often expressed in alveolar rhabdomyosarcoma.14The expression of PAX7-FKHR is associated with a 4-year overall survival (OS) rate of 75%, which is much higher than the 3% survival rate associated with the expression of PAX3-FKHR (P= .0015). Synovial sarcoma may express the fusion of SYT-SSX1 or SYT-SSX2.12Some findings support the prognostic value of SYT-SSX fusion, while others invalidate it.15-17
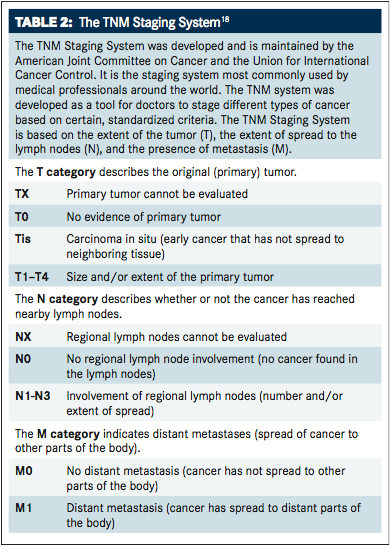
Staging and Prognosis
Staging of STS is based on the American Joint Committee on Cancer (AJCC) classification system (TABLE 2).18In addition to tumor grade, staging considers the depth and size of tumor, the spread to the lymph nodes, and the presence of metastases.
The average 5-year survival rate for patients with STS is approximately 65%, but this can vary with stage and histology.3When the disease is localized, the 5-year survival rate can be >80% or <20% when the disease has metastasized (FIGURE4). Prognosis is usually better when STS is located in the extremities compared with the retroperitoneum.19In an epidemiologic study, Corey et al compared 5-year survival of STS subtypes and found that dermatofibrosarcoma had the highest rate of 5-year survival at 92%.20Well-differentiated liposarcoma also had a high 5-year survival rate (84%), whereas dedifferentiated chondrosarcoma had the lowest rate of 5-year survival (19%). Alveolar rhabdomyosarcoma also had a low rate of 5-year survival (20%).
Gholam Contrasts Lenvatinib With Other Options in Child-Pugh B HCC
December 21st 2024During a Case-Based Roundtable® event, Pierre Gholam, MD, discussed how post hoc and real-world analyses build upon the limited available trial data for treating patients with unresectable hepatocellular carcinoma with Child-Pugh B status.
Read More
Oncologists Discuss a Second-Generation BTK for Relapsed/Refractory CLL
December 18th 2024During a Case-Based Roundtable® event, Daniel A. Ermann, MD, discussed evaluation and treatment for a patient with relapsed chronic lymphocytic leukemia after receiving venetoclax and obinutuzumab.
Read More