Ramucirumab Approved by FDA for Gastric and GEJ Adenocarcinoma
The FDA has approved ramucirumab as a treatment for patients with unresectable gastric cancer or GEJ adenocarcinoma following fluoropyrimidine- or platinum-containing therapy, based on a significant extension in overall survival (OS).
Source: Dr. Lance Liotta Laboratory, The Web site of the National Cancer Institute (http://www.cancer.gov).
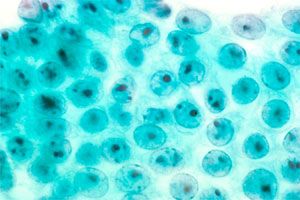
Reactive human stomach cells, that are non-malignant.Source: Dr. Lance Liotta Laboratory, The Web site of the National Cancer Institute (http://www.cancer.gov).
The FDA has approved the VEGFR-2 inhibitor ramucirumab (Cyramza) as a treatment for patients with unresectable gastric cancer or gastroesophageal junction (GEJ) adenocarcinoma following fluoropyrimidine- or platinum-containing therapy, based on a significant extension in overall survival (OS).
In the phase III REGARD trial, the median OS was 5.2 months compared to 3.8 months and the median progression-free survival (PFS) was 2.1 months compared to 1.3 months, for ramucirumab compared with placebo, respectively. The FDA also cited the RAINBOW trial, which combined ramucirumab with the chemotherapy paclitaxel. In this study, the median OS with the combination was 9.7 months compared with 7.4 months with paclitaxel alone. The FDA reviewed ramucirumab under its Priority Review program.
Learn more about ramucirumab for gastric cancer > >
“Although the rates of stomach cancer in the United States have decreased over the past 40 years, patients require new treatment options, particularly when they no longer respond to other therapies,” Richard Pazdur, MD, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research, said in a statement. “Cyramza is [a] new treatment option that has demonstrated an ability to extend patients’ lives and slow tumor growth.”
In the REGARD study, 355 patients with advanced gastric cancer or GEJ adenocarcinoma were randomized 2:1 to receive best supportive care plus either ramucirumab (n=238) or placebo (n=117). Ramucirumab was administered intravenously every 2 weeks at 8 mg/kg for a median duration of 8 weeks. The primary endpoint was OS, with secondary endpoints of PFS, overall response rate (ORR), and safety.
According to results published inThe Lancet, the hazard ratio (HR) for OS was 0.776 (5.2 months versus 3.8 months; 95% CI, 0.603-0.998;P= 0.047) and the HR for PFS was 0.483 (9.7 months versus 7.4 months; 95% CI, 0.376-0.620;P< 0.0001). ORR was 3.4% for ramucirumab and 2.6% for placebo, and disease control rates were 48.7% and 23.1%, respectively.
Approximately 75% of patients in the ramucirumab arm were diagnosed with advanced gastric cancer. Following the discontinuation of treatment, 32% of patients in the ramucirumab arm went on to receive chemotherapy compared with approximately 39% of those on placebo.
Ramucirumab was approved with a Boxed Warning regarding increased risk of severe and sometimes fatal hemorrhage. In the study, hypertension was more common in the ramucirumab arm (16% versus 8%). However, all-grade adverse events were similar between the two groups at 94% compared with 88% for ramucirumab and placebo, respectively.
“We have relied on standard chemotherapies for a long time, and we’ve needed targeted agents based on the fundamental biology of stomach cancer,” Charles Fuchs, MD, MPH, director of the Gastrointestinal Cancer Center at the Dana-Farber Cancer Institute and lead investigator of the REGARD trial, said in a statement. “The benefit is modest, but it’s clearly better than what we were previously doing. It’s really impressive that an antibody which had very little side effects could provide a survival benefit.”
Results from the phase III RAINBOW trial were presented at the 2014 Gastrointestinal Cancers Symposium. In this study, 665 patients with GEJ and gastric adenocarcinoma were randomized 1:1 to receive ramucirumab plus paclitaxel (n = 330) or placebo plus paclitaxel (n = 335). Patients enrolled in the study were treated with first-line fluoropyrimidine- or platinum-containing therapy.
Most patients in the study had an ECOG performance status of 0 or 1. Both ramucirumab and placebo were administered in respective cohorts intravenously at 8 mg/kg on days 1 and 15. In both arms, paclitaxel was administered at 80 mg/m2on days 1, 8, and 15 of a 4-week cycle.
The HR for OS was 0.807 (9.7 months versus 7.4 months; 95% CI, 0.678-0.962;P= .0169) and the HR for PFS was 0.635 (4.4 months versus 2.9 months; 95% CI, 0.536-0.752;P< .0001). The median time to progression was 5.5 months versus 3.0 months (P< .0001) and ORR was 28% compared with 16% (P= .0001), for the ramucirumab combination versus paclitaxel alone, respectively. The disease control rate with ramucirumab was 80% compared with 64% with paclitaxel (P< .0001).
Grade 3 or greater neutropenia occurred in 40.7% of patients in the combination arm compared with 18.8% for paclitaxel plus placebo. Rates of febrile neutropenia were 3.1% with the combination compared with 2.4% with paclitaxel plus placebo. Hypertension was 14.1% with the ramucirumab combination compared with 2.4% with paclitaxel alone.










