Important Facts to Know About Prescribing a CAR-T Therapy: A Q&A with Dr. Thomas Martin
The following Q&A interview features Dr. Thomas Martin, a multiple myeloma expert at the University of California, San Francisco (UCSF), where he regularly prescribes CAR-T therapies for patients with relapsed or refractory multiple myeloma after four or more prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody.
Keep reading for key insights about some of the most asked questions about CAR-T therapy and what he believes everyone should know about his experience with one therapy in particular, CARVYKTI® (ciltacabtagene autoleucel), a BCMA-targeted CAR-T therapy from Johnson & Johnson and Legend Biotech.
You’ve been a believer in cell therapies for a few years now. What has your personal experience been like treating patients with these therapies, and particularly with using CARVYKTI®?
Dr. Martin:
Despite recent progress, multiple myeloma remains an incurable disease. Patients typically experience multiple relapses and require novel, diverse treatment options to address the significant unmet need that still exists.1 Given this, the approval of CARVYKTI® for the treatment of patients with relapsed or refractory multiple myeloma who have been previously treated with four or more lines of therapy including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody, is a welcome treatment option. In clinical trials, CARVYKTI® demonstrated powerful efficacy as a one-time infusion with the potential for a treatment-free period in a patient population with highly refractory disease. In fact, approximately 98 percent of patients with heavily pretreated multiple myeloma responded with approximately 78 percent of patients achieving stringent complete response (sCR) in the CARTITUDE-1 clinical trial of ciltacabtagene autoleucel (cilta-cel), the generic name for CARVYKTI®.2 This is really meaningful for these patients. Because multiple myeloma is a relapsing/refractory disease, we are always thinking about what treatment will be next and which patients may benefit from treatment with CARVYKTI®. We often need to start the discussions and begin thinking about a treatment plan one or two lines ahead of where they are currently.
One of the CAR-T therapies I often discuss with my patients is CARVYKTI®, which is made by Johnson & Johnson and Legend Biotech. CARVYKTI® was approved by the FDA in February of 2022 and had a 98 percent response rate in the phase 1b/2 clinical trial used in its approval.2 In my experience since approval, we’ve observed patients with truly deep and durable responses following treatment with CARVYKTI®, similar to those observed in clinical studies, where results showed 78 percent sCR and a median duration of response of more than 21 months, respectively. Patients may experience serious side effects, with 95 percent of patients experiencing cytokine release syndrome (CRS) in the clinical trial.2 Additional serious side effects include neurologic toxicities, HLH/MAS, prolonged and recurrent cytopenias, infections, hypogammaglobulinemia, hypersensitivity reactions, secondary malignancies, and effects on ability to drive and use machines.2
Beyond the data in the trial setting, those of us who treat patients with multiple myeloma are learning about how to use CAR-T therapies in our own practices. Among patients who have relapsed following four or more lines of treatment, including the most common classes of multiple myeloma treatments such as proteasome inhibitors, immunomodulatory agents, and anti-CD38 antibodies, we continue to learn about how we can most effectively match appropriate patients to CAR-T therapy in a complex treatment environment.
How would you describe the treatment journey with CARVYKTI®for your patients? What has been challenging and what has been successful?
What is great about CAR-T therapies in multiple myeloma is that patients who may not have been a candidate for autologous transplantation can still be considered for CAR-T therapy after four or more prior lines of treatment.2 However, CAR-T therapy requires more logistics than any other myeloma therapy, and a great deal of coordination is needed.
It’s also important that we educate patients on the potential side effects. This allows the patient and caregivers to prepare for their treatment and to be ready post infusion.
Once a patient is considered a candidate for CARVYKTI®, several procedures must happen on a tight schedule. The patient will start the treatment process and undergo the T-cell collection (apheresis). After collection, the timing of the pre-CAR-T chemotherapy and cell infusion can be solidified. The CARVYKTI® manufacturing process can take several weeks, during which we may need to control the patient's disease with bridging therapy.
Once the CAR-T cells are manufactured and available at the treatment center, the patient can begin lymphodepletion chemotherapy (LD). Patients will be monitored daily for the first 10 days following the CARVYKTI® infusion at the certified treatment center. Patients will need to remain within the proximity of the certified treatment center for at least 4 weeks following the infusion.2
Additionally, patients are required to stay local for at least the first month with 24/7 caregiver support. For many patients, the most challenging components of CARVYKTI® treatment are the logistics and the social support.
We’ve learned that we must be transparent with the goals of the therapy and its timing and logistics. We must be clear about what is required and how this treatment requires a team effort.
I have found patients are often both nervous about the side effects but also hopeful about the possibility of a treatment-free interval for their multiple myeloma following treatment with CARVYKTI®.
What has been your patients’ experience with CARVYKTI®?
Once my team and the patient have made the decision to treat with CARVYKTI®, we engage with the patient and family and tell them to apply for support from J&J and Legend, which may include assistance with arranging places to stay, paying for housing, and helping their caregivers pay for travel. Patients have commented to me about how this support has left a lasting positive impression. The ongoing communication from the J&J and Legend Biotech teams reduces the patient's stress if they know they have somebody to call if they have an issue. The MyCARVYKTI® patient support program makes a real difference in the treatment journey of patients who qualify.
Additionally, since outcomes in my practice have been in line with the clinical trial results, many of my patients have maintained a response to treatment, allowing them to discontinue other multiple myeloma-related treatments during that time.
There are a lot of steps to manage, and you have the privilege of practicing at a certified treatment center. What recommendations do you have for other healthcare professionals who are considering prescribing CARVYKTI®?
For physicians who want to be prescribers, I recommend that they educate themselves on the treatment and potential adverse events. I would also recommend developing local standard operating procedures on patient selection, bridging therapy, CAR-T treatment, management of toxicities, and guidelines for follow-up. They will also need to educate their staff, including providers, nurses, pharmacists and support personnel that work in oncology, intensive care, emergency, infectious disease, and neurology departments.
One has to think of the patient journey and optimize throughput, as this treatment has many steps and they must occur along a tight timeline. This is one of the biggest challenges at UCSF, optimizing throughput and getting the right patient at the right time such that they can successfully maneuver through collection, bridging, LD, and infusion. Based on conversations with my colleagues, I know we’re all eagerly waiting for more treatment slots and hopefully can utilize this treatment for more patients.
That being said, my experience working with J&J and Legend has been very positive, from slot assignment through follow-up after a patient has received CARVYKTI®. Throughout the process of each order, we have ample communication and support coordinating with the J&J and Legend team on the manufacturing of CARVYKTI®. J&J and Legend have been receptive to feedback, updating their processes and communicating quickly whenever new information was needed by our treatment center.
My advice, and perhaps request for prescribers who refer patients to a certified treatment center for CARVYKTI®, is to start thinking about referrals when patients start their third line of therapy, since patients can sometimes progress quickly after the third line of treatment. We constantly consider what treatment is next, and having CAR-Ts along with bispecific therapies for patients with relapsed or refractory multiple myeloma has changed the conversation for the better.
Overall, it’s important for healthcare providers to identify patients early on who may be a good fit for CARVYKTI® based on the current approved indication to ensure there is a manufacturing slot and supply for them when they are ready for treatment.2
I look forward to continuing to prescribe CARVYKTI® to patients who meet the eligibility criteria for the treatment and I look forward to future data that is coming.
This article is sponsored by Johnson & Johnson and Legend Biotech. Dr. Thomas Martin has previously served as a consultant for Johnson & Johnson and Legend Biotech; he was not compensated for his participation in this article.
CARVYKTI® IMPORTANT SAFETY INFORMATION
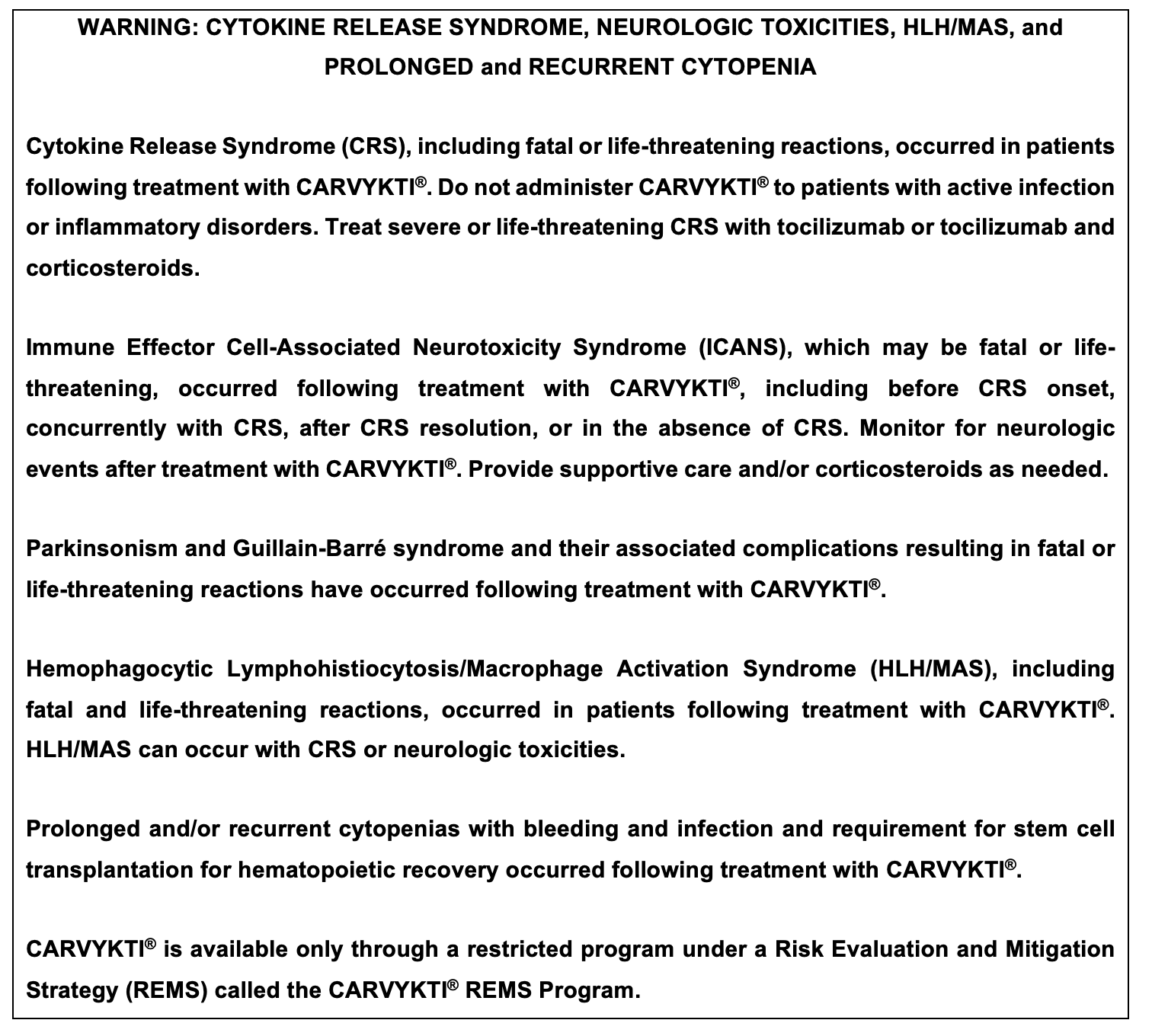
WARNINGS AND PRECAUTIONS
Cytokine Release Syndrome (CRS) including fatal or life-threatening reactions, occurred following treatment with CARVYKTI® in 95% (92/97) of patients receiving ciltacabtagene autoleucel. Grade 3 or higher CRS (2019 ASTCT grade) occurred in 5% (5/97) of patients, with Grade 5 CRS reported in 1 patient. The median time to onset of CRS was 7 days (range: 1-12 days). The most common manifestations of CRS included pyrexia (100%), hypotension (43%), increased aspartate aminotransferase (AST) (22%), chills (15%), increased alanine aminotransferase (ALT) (14%) and sinus tachycardia (11%). Grade 3 or higher events associated with CRS included increased AST and ALT, hyperbilirubinemia, hypotension, pyrexia, hypoxia, respiratory failure, acute kidney injury, disseminated intravascular coagulation and hemorrhage, HLH/MAS, angina pectoris, supraventricular and ventricular tachycardia, malaise, myalgias, increased C-reactive protein, ferritin, blood alkaline phosphatase and gamma-glutamyl transferase.
Identify CRS based on clinical presentation. Evaluate for and treat other causes of fever, hypoxia and hypotension. CRS has been reported to be associated with findings of HLH/MAS, and the physiology of the syndromes may overlap. HLH/MAS is a potentially life-threatening condition. In patients with progressive symptoms of CRS or refractory CRS despite treatment, evaluate for evidence of HLH/MAS. One patient with CRS and suspected HLH/MAS developed a fatal retroperitoneal hemorrhage in the setting of thrombocytopenia, coagulopathy and anticoagulation.
Sixty-nine of 97 (71%) patients received tocilizumab and/or a corticosteroid for CRS after infusion of ciltacabtagene autoleucel. Forty-four (45%) patients received only tocilizumab, of whom 33 (34%) received a single dose and 11 (11%) received more than one dose; 24 patients (25%) received tocilizumab and a corticosteroid, and one patient (1%) received only corticosteroids. Ensure that a minimum of two doses of tocilizumab are available prior to infusion of CARVYKTI®.
Monitor patients at least daily for 10 days following CARVYKTI® infusion at a REMS-certified healthcare facility for signs and symptoms of CRS. Monitor patients for signs or symptoms of CRS for at least 4 weeks after infusion. At the first sign of CRS, immediately institute treatment with supportive care, tocilizumab, or tocilizumab and corticosteroids.
Counsel patients to seek immediate medical attention should signs or symptoms of CRS occur at any time.
Neurologic toxicities, which may be severe, life-threatening or fatal, occurred following treatment with CARVYKTI®. Neurologic toxicities included ICANS, neurologic toxicity with signs and symptoms of parkinsonism, Guillain-Barré Syndrome, immune mediated myelitis, peripheral neuropathies, and cranial nerve palsies. Counsel patients on the signs and symptoms of these neurologic toxicities, and on the delayed nature of onset of some of these toxicities. Instruct patients to seek immediate medical attention for further assessment and management if signs or symptoms of any of these neurologic toxicities occur at any time.
Overall, one or more subtypes of neurologic toxicity described below occurred following ciltacabtagene autoleucel in 26% (25/97) of patients, of which 11% (11/97) of patients experienced Grade 3 or higher events. These subtypes of neurologic toxicities were also observed in two ongoing studies.
Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS): Patients may experience fatal or life-threatening ICANS following treatment with CARVYKTI®, including before CRS onset, concurrently with CRS, after CRS resolution, or in the absence of CRS. ICANS occurred in 23% (22/97) of patients receiving ciltacabtagene autoleucel including Grade 3 or 4 events in 3% (3/97) and Grade 5 (fatal) events in 2% (2/97). The median time to onset of ICANS was 8 days (range 1-28 days). All 22 patients with ICANS had CRS. The most frequent (≥5%) manifestation of ICANS included encephalopathy (23%), aphasia (8%) and headache (6%).
Monitor patients at least daily for 10 days following CARVYKTI® infusion at the REMS-certified healthcare facility for signs and symptoms of ICANS. Rule out other causes of ICANS symptoms. Monitor patients for signs or symptoms of ICANS for at least 4 weeks after infusion and treat promptly. Neurologic toxicity should be managed with supportive care and/or corticosteroids as needed.
Parkinsonism: Of the 25 patients in the CARTITUDE-1 study experiencing any neurotoxicity, five male patients had neurologic toxicity with several signs and symptoms of parkinsonism, distinct from immune effector cell-associated neurotoxicity syndrome (ICANS). Neurologic toxicity with parkinsonism has been reported in other ongoing trials of ciltacabtagene autoleucel. Patients had parkinsonian and non-parkinsonian symptoms that included tremor, bradykinesia, involuntary movements, stereotypy, loss of spontaneous movements, masked facies, apathy, flat affect, fatigue, rigidity, psychomotor retardation, micrographia, dysgraphia, apraxia, lethargy, confusion, somnolence, loss of consciousness, delayed reflexes, hyperreflexia, memory loss, difficulty swallowing, bowel incontinence, falls, stooped posture, shuffling gait, muscle weakness and wasting, motor dysfunction, motor and sensory loss, akinetic mutism, and frontal lobe release signs. The median onset of parkinsonism in the 5 patients in CARTITUDE-1 was 43 days (range 15-108) from infusion of ciltacabtagene autoleucel.
Monitor patients for signs and symptoms of parkinsonism that may be delayed in onset and managed with supportive care measures. There is limited efficacy information with medications used for the treatment of Parkinson’s disease, for the improvement or resolution of parkinsonism symptoms following CARVYKTI® treatment.
Guillain-Barré Syndrome: A fatal outcome following Guillain-Barré Syndrome (GBS) has occurred in another ongoing study of ciltacabtagene autoleucel despite treatment with intravenous immunoglobulin (IVIG). Symptoms reported include those consistent with Miller-Fisher variant of GBS, encephalopathy, motor weakness, speech disturbances and polyradiculoneuritis.
Monitor for GBS. Evaluate patients presenting with peripheral neuropathy for GBS. Consider treatment of GBS with supportive care measures and in conjunction with immunoglobulin and plasma exchange, depending on severity of GBS.
Immune Mediated Myelitis: Grade 3 myelitis has occurred 25 days following treatment in another ongoing study. Symptoms reported included hypoesthesia of the lower extremities and the lower abdomen with impaired sphincter control. Symptoms improved with the use of corticosteroids and intravenous immunoglobulin. Myelitis was ongoing at the time of death from other cause.
Peripheral Neuropathy: Six patients in CARTITUDE-1 developed peripheral neuropathy. These neuropathies presented as sensory, motor or sensorimotor neuropathies. Median time of onset of symptoms was 62 days (range 4-136 days), median duration of peripheral neuropathies was 256 days (range 2-465 days) including those with ongoing neuropathy. Patients who experienced peripheral neuropathy also experienced cranial nerve palsies or GBS in other ongoing trials of ciltacabtagene autoleucel. Monitor patients for signs and symptoms of peripheral neuropathies.
Cranial Nerve Palsies: Three patients (3.1%) experienced cranial nerve palsies in CARTITUDE-1. All three patients had 7th cranial nerve palsy; one patient had 5th cranial nerve palsy as well. Median time to onset was 26 days (range 21-101 days) following infusion of ciltacabtagene autoleucel. Occurrence of 3rd and 6th cranial nerve palsy, bilateral 7th cranial nerve palsy, worsening of cranial nerve palsy after improvement, and occurrence of peripheral neuropathy in patients with cranial nerve palsy have also been reported in ongoing trials of ciltacabtagene autoleucel. Monitor patients for signs and symptoms of cranial nerve palsies. Consider management with systemic corticosteroids, depending on the severity and progression of signs and symptoms.
Hemophagocytic Lymphohistiocytosis (HLH)/Macrophage Activation Syndrome (MAS): Fatal HLH occurred in one patient (1%), 99 days after ciltacabtagene autoleucel. The HLH event was preceded by prolonged CRS lasting 97 days. The manifestations of HLH/MAS include hypotension, hypoxia with diffuse alveolar damage, coagulopathy, cytopenia, and multi-organ dysfunction, including renal dysfunction.
One patient with grade 4 HLH/MAS developed fatal intracerebral and gastrointestinal hemorrhage in the setting of coagulopathy and thrombocytopenia 12 days after treatment in another ongoing study. Patients who develop HLH/MAS have an increased risk of severe bleeding. Monitor hematological parameters in patients with HLH/MAS and transfuse per institutional guidelines.
HLH is a life-threatening condition with a high mortality rate if not recognized and treated early. Treatment of HLH/MAS should be administered per institutional standards.
CARVYKTI® REMS: Because of the risk of CRS and neurologic toxicities, CARVYKTI® is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the CARVYKTI® REMS.
Further information is available at https://www.carvyktirems.com/ or 1-844-672-0067.
Prolonged and Recurrent Cytopenias: Patients may exhibit prolonged and recurrent cytopenias following lymphodepleting chemotherapy and CARVYKTI® infusion. One patient underwent autologous stem cell therapy for hematopoietic reconstitution due to prolonged thrombocytopenia.
In CARTITUDE-1, 30% (29/97) of patients experienced prolonged Grade 3 or 4 neutropenia and 41% (40/97) of patients experienced prolonged Grade 3 or 4 thrombocytopenia that had not resolved by Day 30 following ciltacabtagene autoleucel infusion.
Recurrent Grade 3 or 4 neutropenia, thrombocytopenia, lymphopenia and anemia were seen in 63% (61/97), 18% (17/97), 60% (58/97), and 37% (36/97) after recovery from initial Grade 3 or 4 cytopenia following infusion. After Day 60 following ciltacabtagene autoleucel infusion, 31%, 12% and 6% of patients had a recurrence of Grade 3 or higher lymphopenia, neutropenia and thrombocytopenia, respectively, after initial recovery of their Grade 3 or 4 cytopenia. Eighty-seven percent (84/97) of patients had one, two, or three or more recurrences of Grade 3 or 4 cytopenias after initial recovery of Grade 3 or 4 cytopenia. Six and 11 patients had Grade 3 or 4 neutropenia and thrombocytopenia, respectively, at the time of death.
Monitor blood counts prior to and after CARVYKTI® infusion. Manage cytopenias with growth factors and blood product transfusion support according to local institutional guidelines.
Infections: CARVYKTI® should not be administered to patients with active infection or inflammatory disorders. Severe, life-threatening or fatal infections occurred in patients after CARVYKTI® infusion.
Infections (all grades) occurred in 57 (59%) patients. Grade 3 or 4 infections occurred in 23% (22/97) of patients; Grade 3 or 4 infections with an unspecified pathogen occurred in 17%, viral infections in 7%, bacterial infections in 1%, and fungal infections in 1% of patients. Overall, four patients had Grade 5 infections: lung abscess (n=1), sepsis (n=2) and pneumonia (n=1).
Grade 5 infections reported in other studies include bronchopulmonary aspergillosis, pneumocystis jirovecii pneumonia, and CMV colitis (with HSV-1 hepatitis). Another patient developed mycotic aneurysm due to cerebral aspergillosis and died of subarachnoid hemorrhage.
Monitor patients for signs and symptoms of infection before and after CARVYKTI® infusion and treat patients appropriately. Administer prophylactic, pre-emptive and/or therapeutic antimicrobials according to the standard institutional guidelines. Febrile neutropenia was observed in 10% of patients after ciltacabtagene autoleucel infusion, and may be concurrent with CRS. In the event of febrile neutropenia, evaluate for infection and manage with broad-spectrum antibiotics, fluids and other supportive care, as medically indicated.
In a randomized controlled study of relapsed or refractory multiple myeloma (CARTITUDE- 4), patients treated with ciltacabtagene autoleucel had an increased rate of fatal COVID19 infections compared to the standard therapy arm. Counsel patients on the importance of prevention measures. Follow institutional guidelines for the vaccination and management of immunocompromised patients with COVID-19.
Viral Reactivation: Hepatitis B virus (HBV) reactivation, in some cases resulting in fulminant hepatitis, hepatic failure and death, can occur in patients with hypogammaglobulinemia. Perform screening for Cytomegalovirus (CMV), HBV, hepatitis C virus (HCV), and human immunodeficiency virus (HIV), or any other infectious agents if clinically indicated in accordance with clinical guidelines before collection of cells for manufacturing. Consider antiviral therapy to prevent viral reactivation per local institutional guidelines/clinical practice.
Hypogammaglobulinemia was reported as an adverse event in 12% (12/97) of patients; laboratory IgG levels fell below 500 mg/dL after infusion in 92% (89/97) of patients. Monitor immunoglobulin levels after treatment with CARVYKTI® and administer IVIG for IgG <400 mg/dL. Manage per local institutional guidelines, including infection precautions and antibiotic or antiviral prophylaxis.
Use of Live Vaccines: The safety of immunization with live viral vaccines during or following CARVYKTI® treatment has not been studied. Vaccination with live virus vaccines is not recommended for at least 6 weeks prior to the start of lymphodepleting chemotherapy, during CARVYKTI® treatment, and until immune recovery following treatment with CARVYKTI®.
Hypersensitivity Reactions have occurred in 5% (5/97) of patients following ciltacabtagene autoleucel infusion. Serious hypersensitivity reactions, including anaphylaxis, may be due to the dimethyl sulfoxide (DMSO) in CARVYKTI®. Patients should be carefully monitored for 2 hours after infusion for signs and symptoms of severe reaction. Treat promptly and manage appropriately according to the severity of the hypersensitivity reaction.
Secondary Malignancies: Patients may develop secondary malignancies. Monitor life-long for secondary malignancies. In the event that a secondary malignancy occurs, contact Janssen Biotech, Inc., at 1-800-526-7736 for reporting and to obtain instructions on collection of patient samples for testing of secondary malignancy of T cell origin.
Effects on Ability to Drive and Use Machines: Due to the potential for neurologic events, including altered mental status, seizures, neurocognitive decline, or neuropathy, patients are at risk for altered or decreased consciousness or coordination in the 8 weeks following CARVYKTI® infusion. Advise patients to refrain from driving and engaging in hazardous occupations or activities, such as operating heavy or potentially dangerous machinery during this initial period, and in the event of new onset of any neurologic toxicities.
ADVERSE REACTIONS
The most common non-laboratory adverse reactions (incidence greater than 20%) are pyrexia, cytokine release syndrome, hypogammaglobulinemia, hypotension, musculoskeletal pain, fatigue, infections of unspecified pathogen, cough, chills, diarrhea, nausea, encephalopathy, decreased appetite, upper respiratory tract infection, headache, tachycardia, dizziness, dyspnea, edema, viral infections, coagulopathy, constipation, and vomiting. The most common laboratory adverse reactions (incidence greater than or equal to 50%) include thrombocytopenia, neutropenia, anemia, aminotransferase elevation, and hypoalbuminemia.
Please read full Prescribing Information, including Boxed Warning, for CARVYKTI®.
cp-258862v6
References
- Wang, et al. Treatment patterns and overall survival of patients with double-class and triple-class refractory multiple myeloma: a US electronic health record database study. Leukemia & Lymphoma. 2023;64(2):398-406. https:/doi.org/10.1080/10428194-2022.2140284.
- CARVYKTI® [Prescribing Information]. Horsham, PA: Janssen Biotech, Inc.