World Ovarian Cancer Day: Education and Advances in Treatment
For World Ovarian Cancer Day, Eirwen M. Miller, MD, discussed the current state of ovarian cancer treatment, new developments in the space, and unmet needs.
Eirwen M. Miller, MD

Due to its vague symptoms and often late-stage diagnoses, ovarian cancer remains one of the most challenging cancers to diagnose and treat. However, the treatment landscape of ovarian cancer has seen rapid advancements in recent years, especially with the introduction of PARP inhibitors and ongoing research into novel therapies like antibody-drug conjugates (ADCs).
In an interview with Targeted OncologyTM for World Ovarian Cancer Day, Eirwen M. Miller, MD, gynecologic oncologist at Allegheny Health Network (AHN), discussed the current state of ovarian cancer treatment, new developments in the space, and unmet needs.
Targeted Oncology: What are some of the biggest challenges in treating ovarian cancer today?
Miller: One of the greatest challenges that we experience is diagnosing ovarian cancer at a treatable stage. The symptoms of ovarian cancer are vague and often not manifested until [the] disease is metastatic. What we would love to find is opportunities for earlier intervention with improved screening strategies. For high-risk women, we do not have great screening strategies that afford us opportunity for early intervention.
One of the big struggles we have right now is diagnosis at an early stage where we have the opportunity for cure. The majority of patients have advanced cancer when they are diagnosed, and as a result, we can treat it and we can achieve some long progression-free and overall survivals, but the opportunity for cure remains relatively low.
How is research on ovarian cancer progressing?
The latest research in ovarian cancer has been robust and rapid. In the 7 years that I have been in practice since fellowship, the standard of care for ovarian cancer has changed in almost every state of the disease. In the upfront setting, we have had multiple randomized phase 3 trials looking at various maintenance strategies which have seen to move our progress forward, particularly in homologous recombination deficient and BRCA mutated cancers with PARP inhibitors, studies looking at the combination of PARP inhibitors with [bevacizumab (Avastin)]. I think, certainly in the frontline setting, our standard of care has changed significantly.
In the platinum-sensitive setting, we conversely have had some withdrawals of indications that have challenged our treatment there. But [we are] looking now at some more novel agents in the platinum-sensitive space, particularly looking at some antibody-drug conjugates for maintenance therapy. The platinum-resistant space for ovarian cancer is often robust with clinical trial options and drug development. We are excited about a handful of antibody-drug conjugates that are being introduced into the space and evaluating what their efficacy is in ovarian cancer and moving them through the clinical trial pipelines.
What are the different treatment options available and how are they chosen for each patient?
It depends on where the patient is in their disease course. As a bread-and-butter upfront treatment remains a combination of surgery and chemotherapy. Whether we are selecting primary debulking surgery or neoadjuvant chemotherapy, we rarely have one without the other, whether that is chemotherapy or surgery, it is almost always a combination of both. We have really moved the state of the science into thinking about maintenance therapy for all patients. There is a rare patient that I think is a reasonable candidate for active surveillance and does not receive any maintenance therapy at all in the upfront setting.
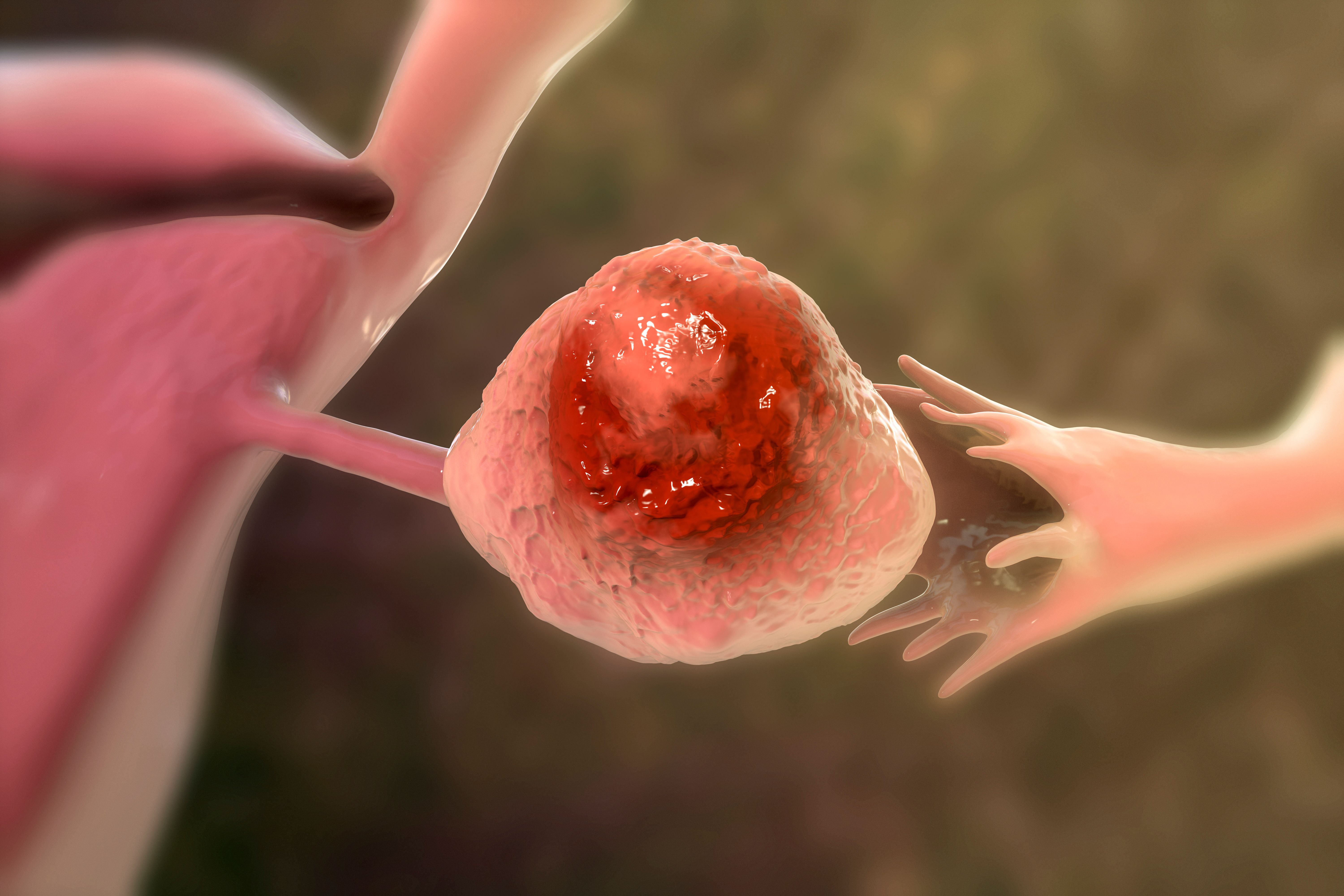
Ovarian cancer: © Dr_Microbe - stock.adobe.com
In the platinum-sensitive setting, it is similar where there is a subset of patients that I think should be carefully selected and considered for a secondary debulking surgery. Almost every patient is going to have an indication for chemotherapy in the second-line setting, and thinking about what our maintenance strategies are there as well.
For the most part, platinum-resistant disease is managed with chemotherapy, but our portfolio of chemotherapy options is changing every day and has made some significant strides. We are using the standard cytotoxic chemotherapy options that we have had for a long time, and the addition of bevacizumab to some of those chemotherapy options based on the AURELIA trial [NCT00976911] published years ago. We now have some data to support the use of immunotherapy with [cyclophosphamide (Cytoxan)] and bevacizumab, so introducing immunotherapy into ovarian cancer space. There is a lot of excitement about antibody-drug conjugates. Specifically, we had mirvetuximab soravtansine-gynx [Elahere] that was FDA-approved for folate receptor alpha high expressing ovarian cancers.
I think that where we are headed is into an era of targeted therapy. When we look at the patients with platinum-resistant disease that are eligible for mirvetuximab, it is limited by the percentage of the population who has an ovarian cancer that is high expressing of folate receptor alpha. So [we will be] looking at some alternative targets like TROP2 antibody-drug conjugates to see if we can broaden the number of patients where we have a targeted therapy option for them.
What are your thoughts on incorporating newer approaches like targeted therapies and immunotherapy into treatment regimens?
I think immunotherapy in ovarian cancer has been relatively disappointing across the board. We have a good number of phase 3 trials where immunotherapy does not seem to be the slam dunk that it has been in some other disease sites. I think immunotherapy in and of itself is largely disappointing, though there may be some kind of small instances where it may have some efficacy. The antibody-drug conjugates, I think, are going to be a critical part of our ovarian cancer treatment strategies moving forward. Right now, we only have 1 that is FDA approved, but we have a multitude in clinical trials that we are excited to investigate and hopefully bring to market.
Are there any other promising new treatments on the horizon?
There is always a lot in clinical trials and under investigation. We have a current clinical trial open at AHN looking at proteomic signatures, so protein signatures in ovarian cancer with drugs that are targeted, not necessarily towards a specific protein, highly expressed on the tumor cell, but a protein signature within it. That certainly has some promise. We have had, unfortunately, a lot of negative clinical trials in ovarian cancer as well. We talked about ADCs a million times; it is like a buzzword today, but I think that is the area that shows the most promise right now.
For World Ovarian Cancer Day, are there any specific areas where you believe educational efforts regarding ovarian cancer could be improved for oncologists?
I think the educational opportunities that we have are with the patients themselves, linking directly to the women in the population about what those symptoms are. Often the symptoms are vague, the symptoms are kind of upper abdominal and gastrointestinal and are often confused for gastrointestinal disorders. It is not uncommon that I hear a patient telling me [they have] been telling someone for 6 months that [they] have heartburn or [are] bloated. We hear that all the time. I think the opportunities that we have for education are with women, with our patients, and with the doctors that they have established care with for many years. Looking at their primary care physicians at their general OBGYNs that they have been seeing once a year for their annual well woman care, and focusing our education in those places that ovarian cancer symptoms are vague. When all of these symptoms are unexplained, it is worthwhile to keep ovarian cancer in the differential diagnosis, and when things do not make sense, we go looking for them.
Personally, how do you stay up to date on all of these advances in research as there is so much coming out all the time?
The journals that are delivered to the house do not just sit on the coffee table; we have to read them and read the literature as it is released. Certainly, attending national organizational meetings every year [is] critical. Large trials and early phase 1/2 trials are typically presented, and it is important to attend and hear them firsthand. I feel fortunate that at AHN we are actively involved in these clinical trials, enrolling patients, and we have a robust clinical trial portfolio understanding kind of what clinical trials are available at any given time and actively putting those patients on trial. Treating them gives a kind of a personal interest in what the outcomes of that trial are, not only to share with the patients that committed their time and their energy to enrolling on a trial, but also for yourself and advancement of the field. Hopefully participating in this process brings new treatment options to the forefront.
What advice do you have for oncologists wanting to learn more about ovarian cancer and the awareness month?
One of the common things, based on my own practice in the last couple of months, is the importance of a family history when we are seeing our patients. I think the family history can be easily breezed over. But we are learning more about the genetic associations between ovarian cancer and some germline mutations. It is not uncommon that we will see a patient and now we know they have ovarian cancer, but they say their mom had breast cancer, sister had breast cancer, grandma had ovarian cancer, and there was potentially an opportunity for risk reduction for this woman had we flagged her family history and considered the option of genetic testing earlier on in their treatment course. While a minority of ovarian cancers are associated with the germline genetic mutation, it is an opportunity that we have to reduce a woman's risk for what is likely to be a future fatal disease. Symptom education and not underestimating the value of taking a good family history and referring to genetics when [there are] some red flags [is important].
Brain Cancer Awareness Month: Challenges and Innovations in Treatment
May 13th 2024In an interview with Targeted Oncology for Brain Cancer Awareness Month, Theodore Schwartz, MD, discussed the challenges of targeting brain tumors, emerging therapies, and strategies to overcome the blood-brain barrier.
Read More
SELECT Trial Establishes Lenvatinib’s Role in RAI-Refractory DTC
May 2nd 2024In an interview with Targeted Oncology, Lori J. Wirth, MD, delved into how the data from SELECT signals lenvatinib effectiveness as a frontline therapy for patients with RAI-refractory differentiated thyroid cancer.
Read More